
2024-114 State Health Care Staffing Contracts
Contract Workers Are a Small but Growing Proportion of Three State Facilities’ Workforces
Published: December 4, 2025Report Number: 2024-114
December 4, 2025
2024‑114
The Governor of California
President pro Tempore of the Senate
Speaker of the Assembly
State Capitol
Sacramento, California 95814
Dear Governor and Legislative Leaders:
As directed by the Joint Legislative Audit Committee, my office conducted an audit of the California Department of Corrections and Rehabilitation (CDCR) and its Salinas Valley State Prison facility, the Department of Developmental Services (DDS) and its Porterville Developmental Center facility, and the Department of State Hospitals (DSH) and its Atascadero State Hospital facility. Our assessment focused on the three departments’ use of health care staffing contracts at these facilities, and we determined that although contract workers make up a small portion of medical and mental health staffing, the facilities have increasingly used them to address their growing number of staff vacancies.
Since July 2019, vacancy rates have increased to 30 percent at Atascadero, 36 percent at Porterville, and more than 50 percent at Salinas Valley. Although the facilities have engaged in multiple recruitment strategies, they have not evaluated the success of their efforts to determine which are most effective. To help address vacancies, each facility has significantly increased its use of contract workers: Atascadero by 79 percent, Porterville by 172 percent, and Salinas Valley by 46 percent. Contract workers generally cost the State more than state employees in the same job classifications, and the shorter tenure of contract workers presents challenges for facilities because of the training necessary to ensure that the contract workers are prepared to provide appropriate care to the facilities’ patient populations.
The many staff vacancies have resulted in each facility realizing significant savings from fiscal year 2019–20 through 2024–25: about $247 million for Atascadero, $188 million for Salinas Valley, and $157 million for Porterville. Nonetheless, neither DSH nor DDS has required staff to evaluate staffing needs annually. Further, none of the three agencies require their facilities to report whether they are meeting shift-staffing minimums, which are critical to ensuring the provision of legally required levels of care. Because of the decades-long difficulties the facilities have had in filling vacant health care positions and a current and projected health care professional shortage, the State should consider facilitating a statewide campaign to draw medical and mental health care workers to California’s civil service.
Respectfully submitted,
GRANT PARKS
California State Auditor
Selected Abbreviations Used in This Report
| CalHR | California Department of Human Resources |
| CCHCS | California Correctional Health Care Services |
| CDCR | California Department of Corrections and Rehabilitation |
| CHA | California Hospital Association |
| DDS | Department of Developmental Services |
| DSH | Department of State Hospitals |
| FTE | Full-time equivalent |
| HCAI | Department of Health Care Access and Information |
| HRSA | Health Resources and Services Administration |
| SAM | State Administrative Manual |
| SCO | State Controller’s Office |
| SPB | State Personnel Board |
Summary
Key Findings and Recommendations
The California Department of Corrections and Rehabilitation (CDCR), the Department of Developmental Services (DDS), and the Department of State Hospitals (DSH) have a responsibility to provide medical and mental health care to individuals who are incarcerated in or committed to the facilities they oversee. To determine the extent to which these departments rely on contract workers rather than state employees to provide this care, the Joint Legislative Audit Committee directed us to examine staffing levels at three facilities: the Department of State Hospitals‑Atascadero (Atascadero), which DSH oversees; the Porterville Developmental Center (Porterville), which DDS oversees; and Salinas Valley State Prison (Salinas Valley), which CDCR oversees. Our review determined the following:
The Three Facilities We Reviewed Have Increasingly Struggled to Fill Vacant Positions
Over the past five years, vacancy rates at all three facilities we reviewed have increased. As of fiscal year 2023–24, the vacancy rate was just over 30 percent at Atascadero, 36 percent at Porterville, and more than 50 percent at Salinas Valley. Most of these vacant positions were in nursing and mental health classifications. Facility staff and employee bargaining unit representatives specifically identified the high‑risk nature of the work, a shortage of health care professionals, and low pay as factors contributing to the high number of vacancies. Facility staff also asserted that they must compete with other state facilities and private hospitals for the same limited pool of potential job candidates. Although the facilities have engaged in a number of recruitment strategies, they generally do not evaluate the success of these efforts to determine which are most effective. Given the decades‑long difficulties the facilities have had in filling vacant health care positions and the current and projected health care professional shortage, the State should consider facilitating a statewide campaign to draw medical and mental health care workers to California’s civil service.
To Address Their Vacancies, the Three Facilities Have Increased Their Use of Contract Workers
Contract workers make up a small portion—from 4 percent to 10 percent—of each facility’s medical and mental health care staffing. However, to address ongoing vacancies, each facility has significantly increased its use of contract workers over the past five years: Atascadero by 79 percent, Porterville by 172 percent, and Salinas Valley by 46 percent. Nearly all contract worker classifications cost the facilities more per hour than their state civil service counterparts, even after taking into account the nonwage costs associated with state civil service employment, such as benefits. Although the contract workers we reviewed possessed the necessary licenses and certifications to work within their classifications, they generally had significantly shorter tenures at each facility than state employees in the same classifications. These shorter tenures can present a challenge for facilities because of the training necessary to ensure that the contract workers are prepared to work with their patient populations and provide appropriate care.
CDCR, DDS, and DSH Have Not Taken Necessary Steps to Ensure That Their Facilities Have Appropriate Staffing Levels
By budgeting staff positions appropriately, departments can request that the Legislature fund the staff necessary to meet their facilities’ operational needs, while not requesting positions they do not require. However, from fiscal years 2019–20 through 2024–25, the three facilities we reviewed had a significant number of vacant positions that they did not cover with either state overtime or contract workers. Moreover, each facility realized significant savings from these vacant positions over the six years: about $247 million for Atascadero, $188 million for Salinas Valley, and $157 million for Porterville. Nonetheless, neither DSH nor DDS has established policies and procedures to ensure that their process for staff budgeting is adequate, such as by including a requirement for staff to evaluate staffing needs at least annually. In addition, DSH, DDS, and CDCR have not formalized a process for facilities to report whether they are meeting shift‑staffing minimums, which are critical to ensuring the provision of legally required levels of care.
Other Areas We Reviewed
In addition, we reviewed staffing logs from the three facilities and found that they used state employees to provide the majority of patient care but filled in shifts with contract workers as necessary. We also conducted interviews with frontline workers to gain insight into their workplace concerns.
To address these findings, we recommended a number of recruiting and retention strategies that the departments and facilities should implement, including exploring the feasibility of maximizing flexible shifts and streamlining their hiring processes. We further recommended that DSH and DDS develop comprehensive policies and procedures for their annual budgeting processes that include the requirement that staff evaluate staffing needs annually and seek adjustments to position authority—the number of positions authorized in the state budget—for each facility as necessary. In addition, we recommended that the departments require their facilities to track, tabulate, and report instances when they fall short of shift‑staffing minimums. Finally, we recommended that the Legislature consider requiring the California Department of Human Resources (CalHR) to facilitate a statewide, cross‑agency collaboration to recruit medical and mental health care staff into California’s civil service and to locations where it is especially difficult to recruit state employees.
Agency Comments
CDCR agreed with our recommendations. DDS and DSH generally agreed with our recommendations, but DDS disagreed with our recommendation that it require its facilities to track and report whether they are meeting required shift-staffing minimums, and DSH disagreed with our recommendation that it evaluate whether offering affordable housing options would improve Atascadero’s ability to recruit new state employees.
Introduction
Background
The three health care facilities we reviewed—Atascadero, Porterville, and Salinas Valley—house individuals who are incarcerated or institutionalized because the courts or those with jurisdiction over those individuals have determined they are a danger to themselves or others, or that they are incompetent to stand trial. State and federal laws require each of these facilities to provide medical and mental health care to the individuals they house. Specifically, the due process clause of the Fourteenth Amendment to the U.S. Constitution and California’s Lanterman‑Petris‑Short Act give individuals who are involuntarily detained the right to prompt medical and mental health care. These laws apply to individuals who are committed to DSH, which oversees Atascadero, and to DDS, which oversees Porterville. Further, the Eighth Amendment of the U.S. Constitution prohibits cruel and unusual punishment of incarcerated individuals. This amendment applies to individuals who are subject to the jurisdiction of CDCR, which oversees Salinas Valley. Individuals subject to the jurisdiction of CDCR include incarcerated individuals who CDCR sends to DSH for psychiatric stabilization. The courts have interpreted a failure to provide adequate medical and mental health care to incarcerated individuals as cruel and unusual punishment.
The Three Facilities Serve Different Populations
The three facilities we reviewed are all in Central California, as Figure 1 shows. Each maintains different licensure types, enabling it to provide medical and mental health care specific to the needs of its population. Atascadero is an acute psychiatric hospital and an intermediate care facility under DSH. It has the largest capacity of the three health care facilities we reviewed, with 1,275 licensed beds. Its all‑male patient population consists mostly of criminal offenders with severe mental illnesses, some of whom were found not guilty by reason of insanity or incompetent to stand trial. Thus, the courts involuntarily committed—either criminally or civilly—these individuals to Atascadero for treatment. A small number of Atascadero’s patients have not been charged with a crime; rather, they are treated under a conservatorship agreement because the courts have determined that their mental illnesses represent a danger to themselves or others.
Figure 1
The Three Central California Facilities Provide Residential Care to Populations With Specific Needs

Source: Websites for DDS, DSH, CDCR, Atascadero, Porterville, Salinas Valley, and California Department of Public Health facility licensing.
A map of California shows the three auditees in Central California.
In the Department of Corrections and Rehabilitation callout bubble, Salinas Valley State Prison is located in Monterey County. Its license type is a Correctional Treatment Center. It has 264 licensed beds. Its population is nearly 2500. Its residents are incarcerated adults.
In the Department of Developmental Services callout bubble, Porterville Developmental Center is located in Tulare County. Its license types are General Acute Care Hospital, Intermediate Care Facility/Developmentally Disabled (ICFDD), ICFDD-Secure Treatment Program (ICFDD-STP). It has 607 licensed beds from 17 acute, 121 ICFDD, and 469 ICFDD-STP. Its population is more than 200. Its residents are developmentally disabled adults.
In the California Department of State Hospitals callout bubble, the Department of State Hospitals-Atascadero is in San Luis Obispo County. Its license types are acute psychiatric hospital and intermediate care facility (ICF). It has 1275 licensed beds from 311 acute and 964 ICF. Its population is more than 1000. Its residents are adults with severe mental illnesses.
Porterville is licensed as a general acute care hospital and as an intermediate care facility for developmentally disabled individuals. The courts criminally or civilly commit individuals to Porterville when the courts have determined they are incompetent to stand trial or pose a danger to themselves or others. DDS oversees the Porterville facility, which has 607 licensed beds. Although Porterville has the physical space to accommodate 607 patients, state law only allows individuals to be admitted to the facility when the population falls below 211 persons.1
Salinas Valley is a state prison that houses incarcerated adults. Within the prison, CDCR, through its California Correctional Health Care Services (CCHCS) division, operates a licensed correctional treatment center with a mental health treatment program. Although Salinas Valley is the largest facility we reviewed by total population, it has the least number of licensed health care beds at 264 because it is not a hospital and only a portion of the facility is designated for medical and mental health care.
All Three Departments Have Been Involved in Litigation Regarding Medical and Mental Health Care Staffing
Dating back decades, the State has been involved in a number of lawsuits regarding its failure to meet minimum medical and mental health care staffing requirements at health care facilities that state agencies operate. In particular, ongoing federal court orders mandate CDCR and its facilities to fill 90 percent or more of certain mental health care positions. In 2023, the court ordered the State to pay monthly fines for noncompliance with mandated mental health staffing levels. As of 2025, CDCR had incurred more than $95 million in accumulated fines, as Figure 2 shows.
Figure 2
For 35 Years, CDCR Has Not Provided Adequate Medical and Mental Health Care
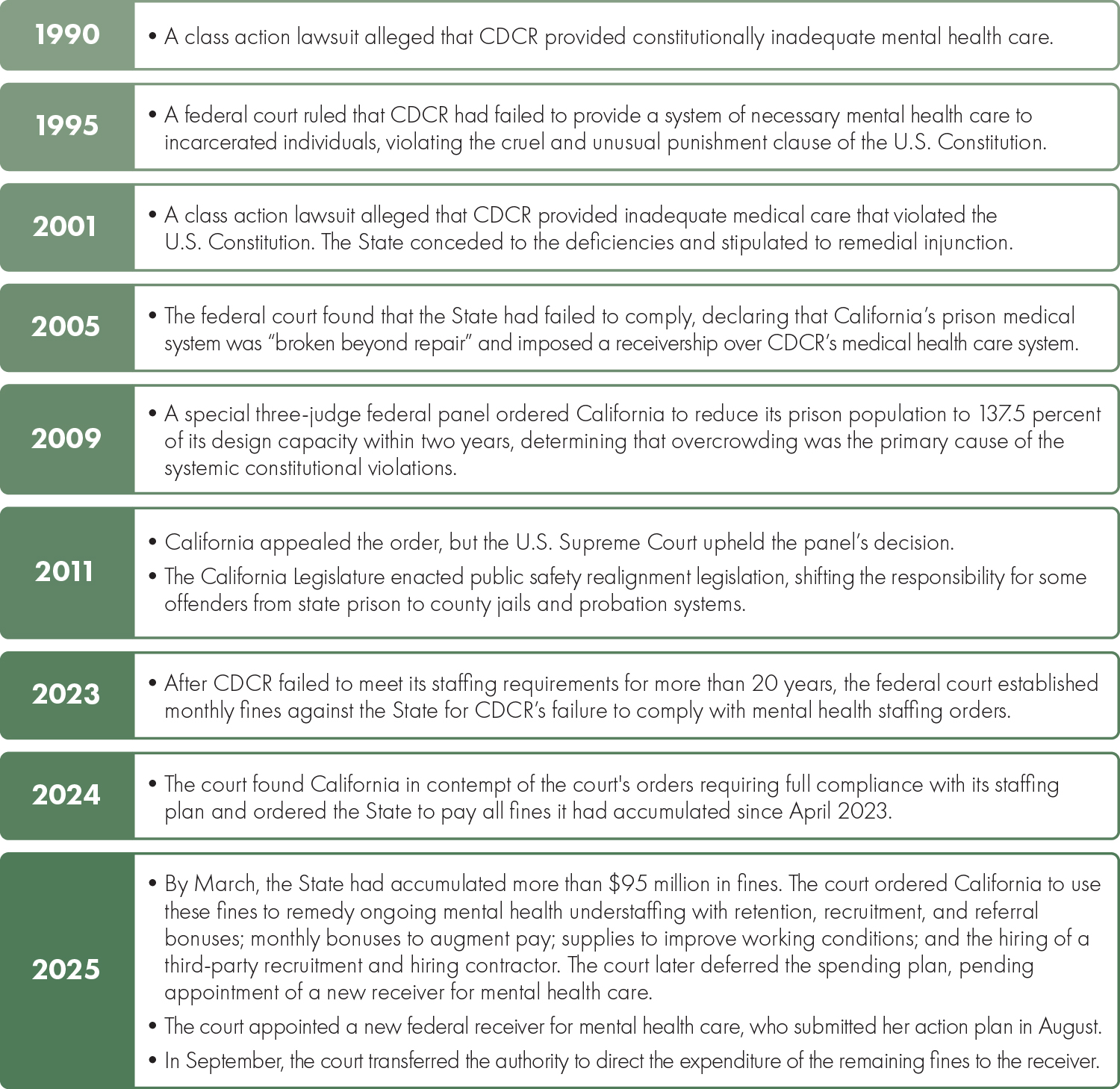
Source: Various court documents related to Coleman v. Brown and Plata v. Newsom court cases.
• 1990: A class action lawsuit alleged that CDCR provided constitutionally inadequate mental health care.
• 1995: A federal court ruled that CDCR had failed to provide a system of necessary mental health care to incarcerated individuals, violating the cruel and unusual punishment clause of the U.S. Constitution.
• 2001: A class action lawsuit alleged that CDCR provided inadequate medical care that violated the U.S. Constitution. The State conceded to the deficiencies and stipulated to remedial injunction.
• 2005: The federal court found that the State had failed to comply, declaring that California’s prison medical system was “broken beyond repair” and imposed a receivership over CDCR’s medical health care system.
• 2009: A special three-judge federal panel ordered California to reduce its prison population to 137.5 percent of its design capacity within two years, determining that overcrowding was the primary cause of the systemic constitutional violations.
• 2011: California appealed the order, but the U.S. Supreme Court upheld the panel’s decision. Also, the California Legislature enacted public safety realignment legislation, shifting the responsibility for some offenders from state prison to county jails and probation systems.
• 2023: After CDCR failed to meet its staffing requirements for more than 20 years, the federal court established monthly fines against the State for CDCR’s failure to comply with mental health staffing orders.
• 2024: The court found California in contempt of the court’s orders requiring full compliance with its staffing plan and ordered the State to pay all fines it had accumulated since April 2023.
• 2025: By March, the State had accumulated more than $95 million in fines. The court ordered California to use these fines to remedy ongoing mental health understaffing with retention, recruitment, and referral bonuses; monthly bonuses to augment pay; supplies to improve working conditions; and the hiring of a third-party recruitment and hiring contractor. The court later deferred the spending plan, pending appointment of a new receiver for mental health care. The court appointed a new federal receiver for mental health care, who submitted her action plan in August. In September, the court transferred the authority to direct the expenditure of the remaining fines to the receiver.
Both DDS and DSH have also been involved in litigation for failing to provide adequate mental health care staffing. Specifically, a 1981 court order required the facilities that the two departments oversee to post in a place that is visible to level‑of‑care staff of each unit and ward their minimum shift‑staffing requirements. In addition, the court order required that the facilities track, tabulate, and report quarterly to their department headquarters the shifts and number of staff by which they fell short. The court order established a best practice to ensure accountability, increase transparency, and allow for the appropriate oversight of mandatory staffing ratios.
The Civil Service Mandate Requires State Agencies to Justify Their Use of Contract Workers Instead of State Employees
A civil service mandate generally prohibits state agencies from contracting with private entities to perform work that the State has historically and customarily performed using the state civil service employees (state employees). This mandate essentially requires state agencies to hire state employees rather than contracting for services unless exempted under state law. Nonetheless, state law provides some exceptions under which agencies may use personal services contracts. In this report, we discuss two provisions of Government Code Section 19130, specifically paragraphs (3) and (10) of subdivision (b) of that section. The first provision applies when the contracted services are not available within civil service. The second applies when the services are of such an urgent, temporary, or occasional nature that the delay inherent in hiring under civil service would frustrate their very purpose.
Personal services contracts are subject to oversight by the State Personnel Board (SPB). The SPB enforces civil service statutes, makes determinations regarding probationary periods and classifications, adopts other civil service rules, and reviews disciplinary actions. In addition, if a state agency cites one of the above‑described provisions as justification when entering a personal services contract, any employee organization that represents state employees can request the SPB to review that contract to determine its adequacy. For example, in 2019, at the request of an employee organization, the SPB reviewed a CDCR contract for six contracted classifications. The SPB approved the contract for two of the classifications but disapproved it for the other four, finding that CDCR either did not demonstrate reasonable and good faith efforts to recruit civil service employees or failed to establish the needed number of civil service positions in those classifications.
Audit Results
- The Three Facilities We Reviewed Have Increasingly Struggled to Fill Vacant Positions
- To Address Their Vacancies, the Three Facilities Have Increased Their Use of Contract Workers
- CDCR, DDS, and DSH Have Not Taken Necessary Steps to Ensure That Their Facilities Have Appropriate Staffing Levels
The Three Facilities We Reviewed Have Increasingly Struggled to Fill Vacant Positions
Key Points
- Vacancy rates at all three of the facilities we reviewed have increased since fiscal year 2019–20. As of fiscal year 2023–24, their vacancy rates for health care positions ranged from just over 30 percent at Atascadero to more than 50 percent at Salinas Valley. Their vacancy rates for psychiatrist and other mental health positions were especially high—often exceeding 50 percent.
- The facilities face several barriers to recruiting new state employees. Each is located in a small city, surrounded by rural areas, in a county with a shortage of health care professionals. The facilities must compete with private sector hospitals, contract staffing agencies, and other nearby state facilities for a limited number of trained job candidates.
- Although the facilities have taken some steps to broaden their recruiting efforts, they could take additional action to make themselves more attractive to potential job candidates, such as offering more scheduling flexibility. The facilities and the departments that oversee them evaluate the results of certain recruitment efforts but could perform additional analysis to determine which of those efforts are the most effective.
In Recent Years, All Three Facilities Have Experienced Significant, Growing Vacancy Rates
Overall, vacancy rates for medical and mental health positions at each of the three facilities we reviewed increased from fiscal years 2019–20 through 2023–24. Vacancy rates can be impacted by a variety of factors, including an increased or decreased number of authorized positions, difficulty filling positions, and staff attrition. As Figure 3 shows, all three facilities had a vacancy rate of 30 percent or more during fiscal year 2023–24, with Salinas Valley having the highest vacancy rate. Salinas Valley’s vacancy rate for medical and mental health care employees increased by 62 percent during our audit period, with more than half of its medical and mental health positions vacant in fiscal year 2023–24. Atascadero had a vacancy rate that was a little more than 30 percent in fiscal year 2023–24, a nearly 39 percent increase from fiscal year 2019–20. Specifically, from fiscal years 2021–22 to 2023–24, Atascadero increased its authorized positions by more than 50, and during that same time frame it lost more than 90 staff to attrition. Although Porterville’s vacancy rate increased only by roughly 6 percent during our review period, 36 percent of its medical and mental health positions were vacant during fiscal year 2023–24.
Figure 3
The Three Facilities’ Vacancy Rates for Medical and Mental Health Care Positions Increased Overall
Fiscal Years 2019–20 Through 2023–24
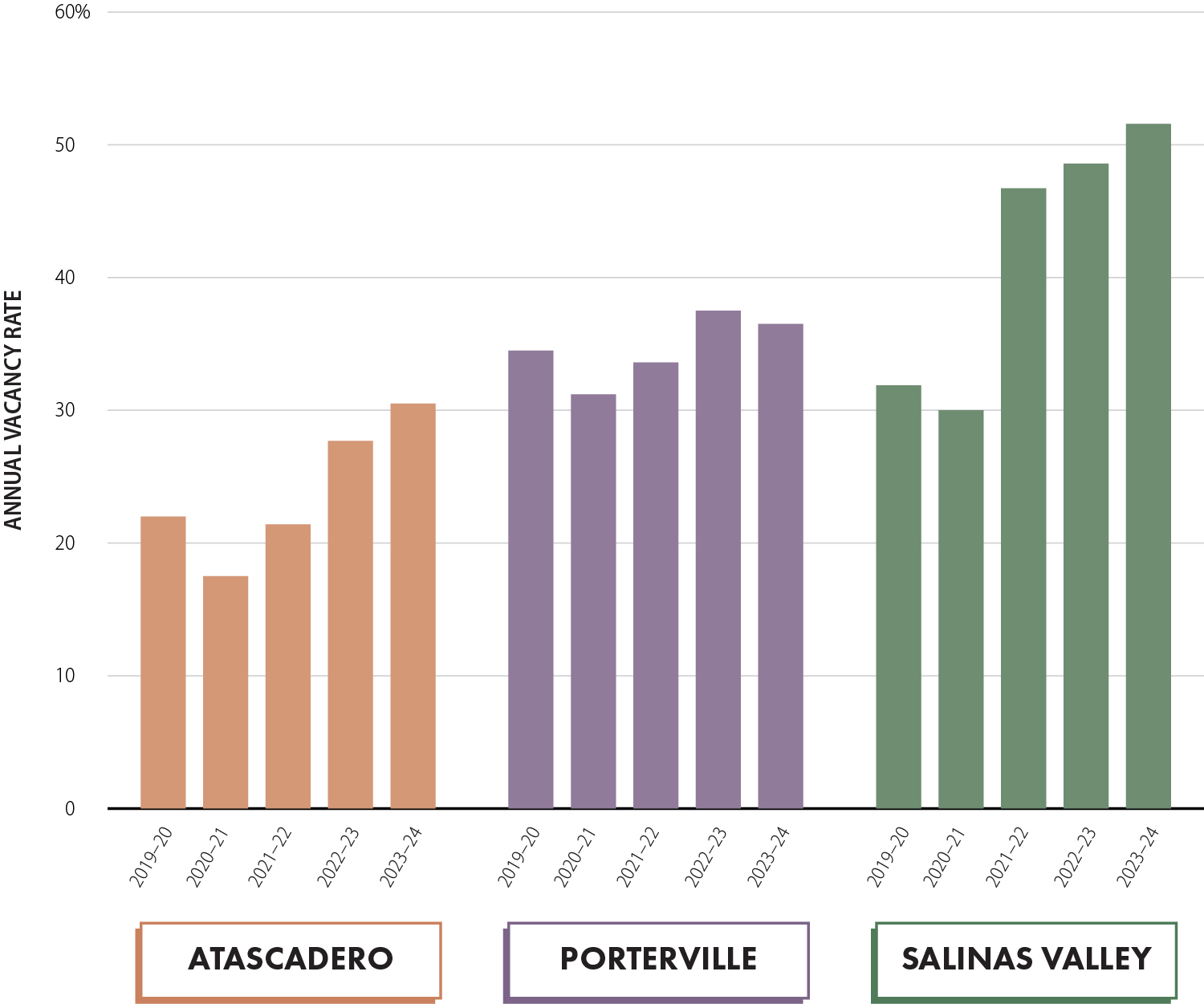
Source: Analysis of State Controller’s Office (SCO) vacancy data, Porterville’s monthly staffing reports, and CDCR’s monthly staffing reports.
Column charts for the three facilities between fiscal years 2019 to 2020 through 2023 to 2024.
At Atascadero, the vacancy rate in 2019 to 2020 was over 20 percent. In 2020 to 2021, the vacancy rate decreased to under 20 percent. In 2021 to 2022 the vacancy rate increased to over 20 percent. In 2022 to 2023, the vacancy rate increased to near 30 percent. In 2023 to 2024 the vacancy rate increased to over 30 percent.
At Porterville, the vacancy rate in 2019 to 2020 was between 30 and 40 percent. In 2020 to 2021, it decreased to just over 30 percent. In 2021 to 2022 it increased to between 30 and 40 percent. In 2022 to 2023, it increased just under 40 percent. In 2023 to 2024 it decreased slightly still above 30 percent.
At Salinas Valley, the vacancy rate in 2019 to 2020 was above 30 percent. In 2020 to 2021, it decreased to 30 percent. In 2021 to 2022, it increased to between 40 and 50 percent. In 2022 to 2023, it increased just under 50 percent. In 2023 to 2024, it increased over 50 percent.
To evaluate trends and compare staffing levels among the facilities, we judgmentally grouped similar job classifications into five main groupings—mental health, nursing, primary care, psychiatry, and other—as the text box shows. As Table 1 indicates, during fiscal year 2023–24, positions in the psychiatry grouping had the highest vacancy rate at Atascadero and the second highest vacancy rate at Porterville and Salinas Valley. During fiscal year 2023–24, Salinas Valley and Atascadero also had high vacancy rates in the other mental health grouping, which includes psychologists and social workers. Porterville, on the other hand, experienced its highest vacancy rate during fiscal year 2023–24 in the primary care grouping.
We Categorized Health Care Job Classifications Into Five Groupings
Mental Health: Psychologists, social workers, and marriage and family therapists.
Nursing: Registered nurses, licensed vocational nurses, certified nursing assistants, and psychiatric technicians.
Primary Care: Physicians, surgeons, medical residents, and physician assistants.
Psychiatry: Psychiatrists.
Other: All other medical or mental health professionals, including behavior specialists, dentists, dietetic technicians, lab assistants, pharmacists, physical therapists, radiologic technologists, rehabilitation therapists, respiratory care practitioners, and speech pathologists.
Source: Auditor generated from review of facility classifications.
Note: The job classifications we list here are just a few of the nearly 200 classifications we included in our review.
Although the nursing grouping did not have the highest vacancy rates at any of the three facilities, vacancies in this grouping largely drove all of their overall vacancy rates because about two‑thirds or more of each facility’s medical and mental health care employees work in nursing classifications. Consequently, vacancies in the nursing grouping accounted for 65 percent or more of all vacancies at each of the three facilities during fiscal year 2023–24. In fact, in fiscal year 2023–24, nursing vacancy rates and total vacancy rates at each of the facilities were within 2 percentage points of each other.
Although employee hiring and separation trends were stable for most job classification groupings throughout our audit period, they fluctuated significantly for the nursing grouping at each of the three facilities we reviewed, as Figure 4 shows. Porterville’s executive director stated that many of its staff in the nursing grouping either left when it closed its general treatment area in 2019 or during the COVID‑19 pandemic. Salinas Valley staff stated that the facility eliminated its medical technical assistant classifications in the nursing group in fiscal year 2019–20 and that many of those employees transitioned to correctional job classifications because of higher rates of pay. Although the departments and facilities focused their perspective on challenges in hiring when asked about vacancies, we noted that, despite their recruiting efforts, attrition often outpaced hiring during our audit period, an issue we discuss later in this report. We present the details of vacancies, hiring, separations, and net gains and losses of state employees by facility, position type, and fiscal year in Table B.1 and Table B.2 of Appendix B.
Figure 4
Net Gains and Losses of Nursing Staff Fluctuated Considerably at All Three Facilities
July 2019 Through December 2024

Source: SCO data.
Note: Net gains and losses are based on appointments and separations. Appointments include hires and changes in job classification, while separations include separations from the facility and changes in job classification. If an individual changed from one job classification to another, but remained within the same job category, they were counted as both an appointment and a separation, resulting in no net gain or loss in that grouping.
Three line charts for each facility depicting erratic net change in Nursing staff from July 2019 through December 2024.
At Atascadero, from July 2019 to July 2020 there was an increase of 80 staff. From July 2020 to July 2021, Nursing staff decreased to around 70. From July 2021 through July 2023, Nursing staff increased to just under 80. By July 2023, Nursing staff decreased to just under 60. In July 2024, it increased just under 80. By December 2024, it decreased to around 70. During this same time, the range for all other groups fluctuated less both over and under 0.Three line charts for each facility depicting erratic net change in Nursing staff from July 2019 through December 2024.
At Porterville, from July 2019 to July 2020 there was a decrease in Nursing staff to between negative 20 and negative 25. By July 2021, Nursing staff increased to between negative 15 and negative 10. In July 2022, Nursing staff decreased again to just over negative 15. By July 2023, it increased to nearly 5. From July 2023 to July 2024, Nursing staff decreased to more than negative 15. By December 2024, it decreased to just over negative 20. The range for all other groups remained positive.
At Salinas Valley, from July 2019 to July 2020 there was a net negative change by nearly negative 60 Nursing staff. By July 2021, there was a there was a slight positive net change in staff. By July 2022, there was a net negative change in Nursing staff to around negative 70. By July 2023, there was a net negative change in Nursing staff to around negative 90. This remained steady to July 2024. By December 2024, there was a slight net positive change to just over negative 80 Nursing staff.
Staff at each department asserted that they have used a mix of state employee overtime and contract workers to cover their ongoing vacancies. However, even after accounting for overtime and contract workers’ hours, each facility still had uncovered vacant positions throughout our audit period. Figure 5 shows the number of full‑time equivalent (FTE) positions that were not covered by state employee overtime or contract workers during fiscal year 2023–24. We discuss the departments’ budgeting of positions at the facilities in the final section of this report.
Figure 5
Facilities Used Overtime and Contract Workers to Cover Vacant Authorized Positions
Fiscal Year 2023–24
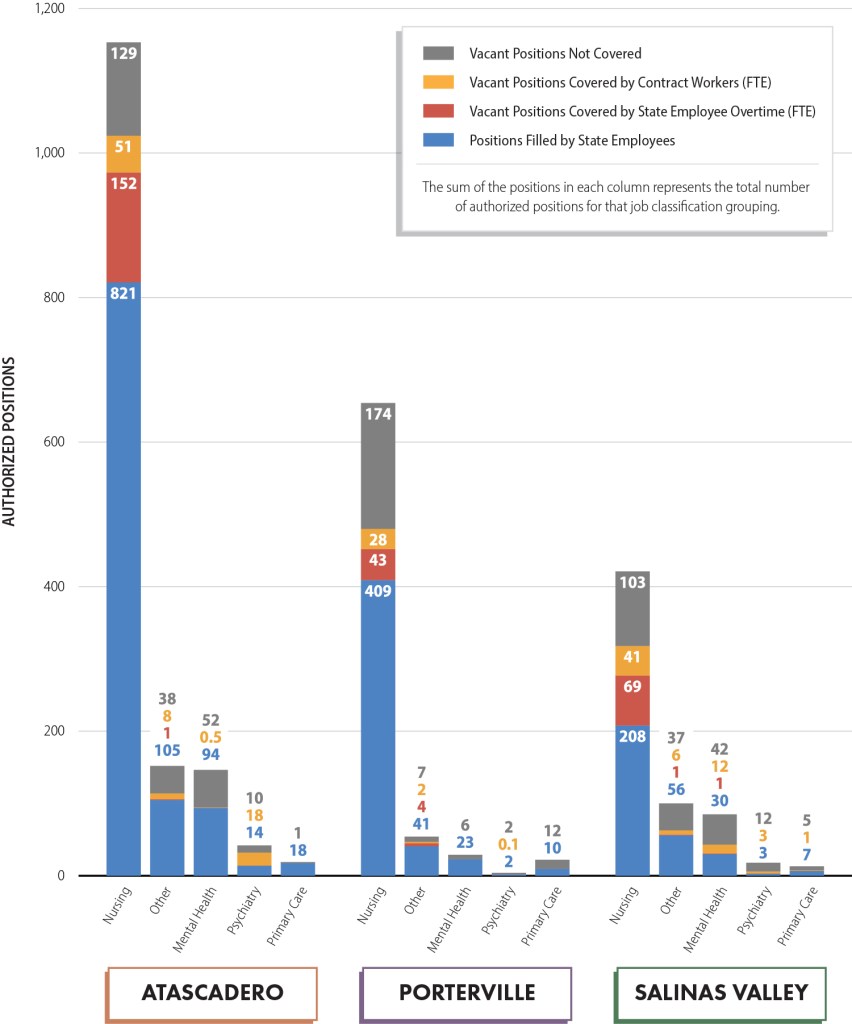
Source: State budget documents, SCO data, Porterville’s monthly staffing reports, CDCR’s monthly staffing reports, and facility invoice data.
Note: Facilities use a combination of voluntary and mandatory overtime, as well as contract workers and retired annuitants, to cover some unfilled shifts caused by vacant positions. We calculated the number of state employee overtime and contract worker full‑time equivalent (FTE) positions by dividing the relevant number of hours worked by 2,080 (52 weeks times 40 hours per week). State employee overtime FTE positions reflect all state employee overtime hours, while contract worker FTE positions reflect all contract worker hours, including regular time and overtime. Because the vacancy data contains only established positions, these results do not include the number of FTE positions filled by retired annuitants and some other temporary positions.
A stacked column chart showing authorized positions for Atascadero, Porterville, and Salinas Valley in the Nursing, Other, Mental Health, Psychiatry, and Primary Care categories. The sum of the positions in each column represents the total number of authorized positions for that job classification grouping. Vacant positions covered by state employee overtime and vacant positions covered by contract workers are both calculated as full-time equivalent (FTE).
At Atascadero, Nursing had 821 positions filled by state employees, 152 vacant positions covered by state employee overtime, 51 vacant positions covered by contract workers, and 129 vacant positions not covered. In the Other grouping, there were 105 positions filled by state employees, 1 vacant position covered by state employee overtime, 8 vacant positions covered by contract workers, and 38 vacant positions not covered. In the Mental Health grouping, there were 94 positions filled by state employees, 0.5 vacant positions covered by contract workers, and 52 vacant positions not covered. In the Psychiatry grouping there were 14 positions filled by state employees, 18 vacant positions covered by contract workers, and 10 vacant positions not covered. In the primary care grouping there were 18 positions filled by state employees and 1 vacant position not covered.
At Porterville, in the Nursing grouping there were 409 positions filled by state employees, 43 vacant positions covered by state employee overtime, 28 vacant positions covered by contract workers, and 174 vacant positions not covered. In the Other grouping there were 41 positions filled by state employees, 4 vacant positions covered by state employee overtime, 2 vacant positions covered by contract workers, and 7 vacant positions not covered. In the Mental Health grouping there were 23 positions filled by state employees and 6 vacant positions not covered. In the Psychiatry grouping there were 2 positions filled by state employees, 0.1 vacant positions covered by state employee overtime, and 2 vacant positions not covered. In the Primary Care grouping there were 10 positions filled by state employees and 12 vacant positions not covered.
At Salinas Valley, in the Nursing grouping there were 208 positions filled by state employees, 69 vacant positions covered by state employee overtime, 41 vacant positions covered by contract workers, and 103 vacant positions not covered. In the Other grouping there were 56 positions filled by state employees, 1 vacant position covered by state employee overtime, 6 vacant positions covered by contract workers, and 37 vacant positions not covered. In the Mental Health grouping there were 30 positions filled by state employees, 1 vacant position covered by state employee overtime, 12 vacant positions covered by contract workers, and 42 vacant positions not covered. In the Psychiatry grouping there were 3 positions filled by state employees, 3 vacant positions covered by contract workers, and 12 vacant positions not covered. In the Primary Care grouping there were 7 positions filled by state employees, 1 vacant position covered by contract workers, and 5 vacant positions not covered.
The Facilities Face a Number of Barriers When Recruiting New State Employees
Each of the facilities we reviewed faces challenges when recruiting staff, including difficult working conditions, a local shortage of health care professionals, and competition with other public facilities, private hospitals, and contract staffing agencies. However, Atascadero, Porterville, and the departments that oversee them have not conducted salary surveys to determine their competitiveness in the marketplace for health care professionals because, according to staff, they lack the necessary funding and resources.
Challenging Work Environments
The facility staff and employee bargaining unit representatives we spoke with identified the high‑risk nature of the work as one of the primary causes of their ongoing vacancies. For example, in October 2025, a riot at Salinas Valley involving about 90 incarcerated individuals resulted in harm to three incarcerated individuals and to one staff member, who was treated for heat exhaustion. Salinas Valley’s chief of mental health stated that some prospective employees may not be interested in working in such an environment, making recruiting staff more difficult. Atascadero and Porterville have similar work environments. In fact, according to DSH, there were nearly 2,900 patient‑on‑patient assaults and more than 2,500 patient‑on‑staff assaults across all of its hospitals in 2020—the most recent year for which published data is available.
Several of the staff we interviewed at Porterville—the only state‑operated facility that serves individuals with mild to moderate intellectual disabilities who have been deemed a danger to themselves or others—described working in conditions in which they are verbally and physically assaulted regularly. According to Porterville’s bargaining unit president, on‑the‑job injuries have led to retirements for some employees. He also asserted that given the unsafe working conditions because of patients who are sometimes violent, the State should offer employees additional compensation while staff work to make the facility safer.
Shortage of Health Care Professionals
Aside from working conditions, a shortage of health care professionals has contributed to the vacancies at the facilities. In a recent report, the California Hospital Association (CHA) stated that the COVID‑19 pandemic delayed education and training for thousands of health care professionals, postponing their entrance into the workforce. CHA further noted that California’s health care pipeline is struggling to keep pace with the demand for services, that 11 million Californians live in an area without enough primary care providers, and that there is a statewide shortage of nurses, physicians, pharmacists, behavioral health professionals, lab scientists, and physical therapists. In addition, the three facilities cited declining enrollment in psychiatric technician programs as a contributing factor for the high vacancies in these positions. According to CDCR staff who recruit for Salinas Valley, the supply of mental health professionals completing school training programs is not enough to meet demand for those professions. A bargaining unit president at Porterville—a senior psychiatric technician with 18 years of state service—explained that enrollment into psychiatric technician programs has been declining since the pandemic.
Moreover, a 2025 report from the Department of Health Care Access and Information (HCAI)—which collects, analyzes, and publishes information about California’s health workforce and identifies areas of the State that are experiencing shortages of health professionals—indicates that more than 33 percent of the State’s psychologists, more than 30 percent of its physicians, and more than 20 percent of its registered nurses were age 60 or older. Some of these older professionals are likely to retire within the next two to five years, further affecting the supply of health care professionals. HCAI data also show that all three facilities we reviewed are in areas with a shortage of psychiatrists and licensed mental health providers. As Table 2 shows, HCAI data indicate that Monterey County has a 31 percent shortage of psychiatrists, San Luis Obispo County has a 39 percent shortage, and Tulare County has a 75 percent shortage.
In addition, HCAI data show that each of the three facilities we reviewed is located in one of California’s nursing shortage areas. According to HCAI, it designates an area as having a nursing shortage when there is a shortage of registered nurses, clinical nurse specialists, public health nurses, and psychiatric mental health nurses within one of California’s counties or, for Los Angeles County, one of its eight service planning areas. Of the 65 total service areas in the State, HCAI identified 48 as having a low, medium, high, or severe nursing shortage designation. Tulare County, where Porterville is located, has a medium nursing shortage area designation. Monterey County, where Salinas Valley is located, and San Luis Obispo County, where Atascadero is located, both have a low nursing shortage designation. According to department and facility staff, all three facilities have struggled to find effective ways to overcome these and other barriers, leaving them with small pools of candidates from which to recruit.
Other Geographical Challenges
The three facilities’ locations present additional challenges for recruiting staff. Each of the three facilities is located in a small city, surrounded by rural areas with small populations, which may not be attractive to some medical and mental health care professionals interested in state employment. The city of Atascadero has a population of about 30,000 residents, while the city of Porterville has about 63,000 residents. The city of Soledad, where Salinas Valley is located, has fewer than 25,000 residents. Staff and bargaining unit representatives at the three facilities identified their rural locations as a barrier to recruitment for candidates who may be looking for a more vibrant lifestyle.
Atascadero is also located in an area with a high cost of living, which makes it more difficult to recruit medical and mental health care professionals. The compensation for many of these professionals may not be sufficient to provide a living wage. In San Luis Obispo County, where Atascadero is located, estimates show that an adult with one child needs to earn $99,396 annually before taxes to make a living wage. Based on the hourly rates the State offers on the CalHR website (CalCareers), we estimate that a starting licensed vocational nurse at Atascadero earns about $65,000, a starting radiology technologist about $79,000, and a starting clinical social worker about $110,000 annually. A bargaining unit president for Atascadero stated that the cost of living in the area is a major barrier to recruitment and retention and that some staff have moved to lower‑cost areas and commute to the facility. Staff at Atascadero similarly asserted that some applicants have turned down jobs because of the costs of housing. The average price of a home in Atascadero is about $830,000, while a small one‑bedroom apartment costs about $2,000 per month.
Competition With Other State and Private Health Care Facilities
Despite working in high‑risk environments, the medical and mental health care state employees we interviewed asserted that they are generally paid less and may receive fewer benefits than similar workers in the private sector or at other state facilities. To obtain perspective and understanding of working conditions and staffing challenges at each of the facilities, we conducted interviews with 21 frontline staff across the three facilities and held numerous meetings and interviews with facility staff and management. For example, Atascadero staff attributed psychiatrist vacancies in part to the fact that the private sector and other facilities can offer psychiatrists higher salaries and more flexibility. Specifically, staff at Atascadero indicated that a nearby private hospital offers signing bonuses of $90,000 to new psychiatrists, while Atascadero can only offer its employees no more than $10,000. Staff also explained that the relocation package that the State allows it to offer is minimal compared to those of private institutions.
The three state facilities must also compete with other state facilities for potential employees. Porterville’s workforce manager stated that her facility faces competition from nearby CDCR facilities. She explained that pay differentials allow CDCR to pay state employees higher wages for the same work that they would perform at Porterville.2 In the same vein, CDCR operates 31 adult state prisons across the State and each correctional facility is competing with other correctional facilities for the same job candidates. All three facilities we reviewed stated that competition with other state facilities and private institutions has made it more difficult for them to recruit medical and mental health care professionals. The text box identifies some of the state facilities and private hospitals located near the three facilities.
Each Facility We Reviewed Competes With Other Nearby Facilities for Health Care Staff
Atascadero:
- Sierra Vista Regional Medical Center
- French Hospital Medical Center
Porterville:
- Avenal State Prison
- California Substance Abuse Treatment Facility
- Kern Valley State Prison
- North Kern State Prison
- Wasco State Prison
- California State Prison, Corcoran
Salinas Valley:
- Correctional Training Facility
- Kaiser Permanente
Source: Interviews with facility staff.
Competition With Staffing Agencies
In addition to competing for potential employees with private hospitals and other state facilities, the three facilities must also contend with staffing agencies, which frequently offer contract workers salary ranges that are higher than the State offers, as Table 3 shows. We did identify some exceptions: for instance, the staffing agencies that contract with Porterville offer lower salary ranges than the State does for certified nursing assistants, registered nurses, licensed vocational nurses, and psychiatric technicians. However, staffing agencies offered higher ranges of pay than the State did for each of the positions we reviewed at one or more of the facilities.
In addition, many staffing agencies offer contract workers benefits similar to those the State offers to its employees. For example, staffing agencies frequently offer health, dental, and vision insurance; malpractice insurance; and retirement plans, including employer‑sponsored retirement savings plans, such as 401(k)s. Some also offered other benefits, such as voluntary identity theft protection plans, transportation assistance, and employee discount programs.
Human resources staff at Atascadero and Porterville and their respective departments acknowledged that civil service salaries are frequently lower than those offered by staffing agencies and stated that these salary differences can negatively affect their recruitment efforts. To address this issue, staff at these departments and facilities have sometimes sought to obtain additional compensation, such as pay differentials, for state employees. To obtain pay differentials, state departments must submit an employee compensation request to the California Department of Human Resources (CalHR). For example, staff at Atascadero explained that they obtained pay differentials of $400 per month for the facility’s psychiatric technicians. However, staff stated that CalHR has frequently denied their requests for reasons that included a lack of state funding. In contrast to DSH and DDS, staff at CDCR asserted that they did not know how much contract workers at Salinas Valley earn and had no perspective on how the differences in the pay for state employees and contract workers might affect their recruitment efforts.
Despite asserting that the State’s salaries may affect their recruitment efforts, staff from Atascadero, Porterville, and their respective departments acknowledged that they have not conducted a formal salary survey to identify differences in state salaries and contract worker salaries. Staff at the two departments stated there may be a benefit to conducting a survey as it could enhance their position when negotiating salary changes with CalHR; however, they explained that they do not have the funding or resources to do so. They also questioned whether the survey results would lead to a change in salaries, given the State’s budgetary constraints. According to DSH staff, when DSH last completed a comprehensive salary survey as part of its supplemental report to the Legislature in fiscal year 2014–15, it did not necessarily result in any salary changes. In contrast, staff at CDCR stated that they purchase annual salary surveys from third‑party entities that the department then uses to develop a salary analysis that compares the salaries earned in the public and private sectors. The last salary analysis that CDCR conducted was in December 2023. CDCR staff use the salary surveys to support their requests to CalHR for salary changes for their staff and explained that salary surveys helped them to support compensation requests for staff at Salinas Valley.
Conducting a salary survey could help Atascadero, Porterville, and their respective departments better understand where they perform well and where they perform poorly in the marketplace for health care professionals, including in comparison to staffing agencies. Further, all three departments have funds from unspent salaries for health care staff that they could use to conduct such surveys. The surveys could also provide budget decision‑makers, including the Legislature and CalHR, with information that is critical to ensuring that the State remains competitive as a potential employer for these essential workers.
Although the Three Facilities Have Made Reasonable Recruiting Efforts, They Can Do More to Assess the Effectiveness of Their Strategies
The three facilities we reviewed have made reasonable efforts to recruit new health care professionals, including placing advertisements in various locations, attending career fairs, and hosting hiring events. However, the facilities and their respective departments have not comprehensively evaluated the effectiveness of these efforts to determine where they should focus resources more effectively. A collaborative, state‑led effort to increase recruitment of health care professionals to California could benefit the facilities and help address the State’s decades‑long history of struggling to fill medical and mental health care positions.
Recruiting Efforts
All three facilities have made significant efforts to recruit medical and mental health care professionals through online job advertisements and in‑person or virtual recruiting events. Each of the facilities advertises in social media, radio, industry magazines, and CalCareers, among other locations. We could not determine the exact number of job postings for each facility on the CalCareers website because many postings are ongoing and some are for multiple positions and facility locations. However, Atascadero had at least 4,063 postings during our audit period, while Porterville and Salinas Valley had at least 654 and 974 postings, respectively. Additionally, each of the three facilities participated in numerous recruiting events most years, as Table 4 shows.
Although the three departments and facilities tracked some of their recruiting efforts during our audit period, they could not demonstrate that they actively compared recruiting strategies to determine which are most effective for getting qualified applicants to apply and ultimately get hired. DSH and CDCR stated that they are both in the process of piloting and implementing systems to evaluate and compare the effectiveness of their various recruiting strategies.3 However, these systems are not yet complete enough to generate meaningful data to guide their efforts. As a result, none of the facilities or departments were able to demonstrate which recruiting strategies were most effective in generating the greatest number of applicants and the greatest hiring percentage. We expected that given the number of vacant positions that the facilities need to fill, the departments and facilities would have already evaluated the effectiveness of their recruiting activities; without this information, they cannot leverage their efforts and focus on those that generate the best results.
Appendix E identifies the number of job applications each of the three facilities received and the number of applicants it interviewed and hired for five different job classifications from calendar years 2019 to 2024.
Recruiting Opportunities
When reviewing the three facilities’ recruiting efforts, we identified several potentially effective strategies that some of the facilities have yet to adopt. For example, of the 49 in‑person or virtual recruiting events that Salinas Valley conducted from 2019 through 2024, 25 were one‑ to three‑day hiring events where interested candidates could apply, interview, and receive a contingent job offer before the event concluded. In 2021, CDCR’s deputy director of human resources developed and implemented these hiring events after identifying a need to streamline the state civil service hiring process. The fact that such condensed events shorten and streamline the hiring process suggests that other facilities should consider implementing something similar.
When we asked human resources staff at Atascadero and Porterville about streamlined hiring events, staff at Porterville stated that they prefer the traditional merit‑based hiring process because they can better ensure that candidates meet the facility’s needs. In contrast, DSH’s recruitment unit manager stated that it has successfully run a similar event for some facility support positions. He explained that DSH is open to expanding streamlined recruiting events to recruit for certain medical and mental health care positions. When we evaluated 37 websites from the staffing agencies with which the three facilities contract, we found that many promote a streamlined hiring process.
The staffing agencies also offer flexible work schedules, referral programs, and résumé assistance, along with the ability to work in various locations. Although the three facilities we reviewed cannot offer the last of these benefits, they could consider whether providing additional flexibility in scheduled shifts is feasible. Several of the state employees we interviewed stated that their current shifts do not allow for work‑life balance. Further, a bargaining unit chapter president for employees at Porterville explained that the bargaining unit has attempted to negotiate such flexibility in the past.
Atascadero offers flexible schedules for some of its level of care staff, such as physicians, psychiatrists, psychologists, and registered nurses. However, Atascadero offers only limited flexible shifts to the positions in its nursing group, which comprises 77 percent of its medical and mental health care staffing. According to staff, Atascadero previously tried to offer 12-hour shifts to state employees in collaboration with bargaining units, but was unsuccessful in finding enough interested employees to accept the schedule. Staff stated that they also found it difficult to make more 12-hour shift options work with operational needs. We recognize that implementing flexible schedules might be difficult; however other 24‑hour facilities in the private sector, such as hospitals, are successful at implementing a variety of flexible schedules. Both CDCR and DDS were also open to the idea of providing additional flexibility. Although we recognize that the departments would need to negotiate with the bargaining units and adhere to all state requirements before making any changes to staff schedules, the departments and facilities could conduct a study to determine whether doing so would be feasible and whether it would improve employee retention and increase the effectiveness of recruitment efforts.
Atascadero and Porterville could also better leverage their existing assets as part of their recruiting efforts. Both facilities have housing available at their locations that they have at times offered to newly hired employees as a recruiting strategy. Porterville has 30 rental properties, and staff stated that there are normally some vacancies. Atascadero has 17 rental properties and eight single rooms for rent, but staff advised that the units are normally full and the leases are for a limited duration. Staff at Atascadero told us that because the housing is normally full, it is of limited value as a recruiting tool. They believe that obtaining or developing additional housing units would require action by the Legislature. However, neither Atascadero nor DSH has explored this option to attract more candidates for the facility.
The State Could Assist the Facilities’ Recruiting Efforts
The problems related to filling medical and mental health positions are not limited to the three facilities we reviewed. The Health Resources and Services Administration (HRSA) within the U.S. Department of Health and Human Services projects a national shortage of more than 187,000 full‑time equivalent physicians and a shortage of 208,000 nurses by 2037. In addition, HRSA projects substantial shortages of mental health providers, including psychologists and psychiatrists. Such nationwide shortages suggest that without significant change, filling medical and mental health care vacancies will likely continue to challenge the State.
Although the departments and facilities can and should implement certain recruitment strategies on their own, we believe that the State could achieve greater efficiency and effectiveness by overhauling and centralizing its efforts to recruit medical and mental health care workers. CalHR could collaborate with various departments to improve the recruitment and hiring of medical and mental health care professionals, similar to the Work for California Hiring and Recruiting Campaign it piloted when seeking employees from the technology sector. This three‑month pilot in 2023 included collaboration between 23 state agencies to increase applications for state jobs, reduce high vacancy rates, and decrease application‑to‑hire time frames. The campaign included dozens of promotional videos, coordinated social media posts, and online interest forms, and it resulted in more than 5.4 million interactions and nearly 8,500 interest forms submitted. The project summary noted there were 1,584 hires, a decrease in vacancy rates, and a reduction in application‑to‑hire time frames for some departments.
The State could adopt a similar but broader campaign through which it centralizes recruiting activities in a cross‑collaboration of agencies and facilities to attract and hire more medical and mental health care professionals. Although the technology pilot project ran for only three months, the severity of nationwide health care shortages and the State’s decades‑long history of struggling to fill medical and mental health care positions suggests that the State should consider conducting an ongoing campaign in this instance. The campaign could continue until the State can achieve and maintain minimal vacancy rates in its medical and mental health care classifications.
We spoke with CalHR’s director about conducting a collaborative cross‑agency recruiting campaign to hire more medical and mental health care professionals into state employment, and she was supportive of CalHR facilitating such an effort. She explained that our proposal for CalHR to incorporate online and in‑person assistance to candidates during the application process, and for it to develop and streamline targeted recruitment activities for difficult to recruit classifications and locations, align with her goals to broaden the support that CalHR offers departments. The director stated that CalHR would need additional resources to facilitate such a campaign. However, she acknowledged that by centralizing some recruiting efforts, the State could improve the efficiency of its hiring activities by reducing some duplicative efforts and competition among the various departments.
As we indicate previously, the extent to which the State’s salaries for medical and mental health care positions reflect the current marketplace is unclear. According to CalHR’s deputy director of fiscal and data management, CalHR performs total compensation analyses on some state occupations. However, these analyses are high‑level and do not include all medical and mental health care classifications. He further explained that it is departments’ responsibility to conduct salary studies for specific classifications, which also consider their facilities’ specific geographical locations and competition. He stated that CalHR offers departments guidance on conducting salary studies so that they can appropriately address compensation concerns and obtain the documentation necessary to seek compensation modifications. Therefore, before engaging in a large recruiting campaign, it would benefit the State to facilitate total compensation analyses of all medical and mental health care positions to ensure that compensation is commensurate and competitive with the private sector. Such an effort could also help ensure that state agencies and facilities are not competing with each other to the State’s overall detriment.
Although CalHR would likely be the most appropriate agency to facilitate, manage, and track the results of such a recruitment campaign, CDCR, DDS, and DSH should collaborate with CalHR to pilot and identify the most effective recruitment strategies. Further, the departments should be responsible for vetting, hiring, and onboarding new applicants.
To Address Their Vacancies, the Three Facilities Have Increased Their Use of Contract Workers
Key Points
- Contract health care workers made up between just 4 and 10 percent of overall staffing levels at each facility. However, each facility has increased its use of contract workers in recent years to help address ongoing vacancies.
- All three state facilities typically incur higher hourly costs for contract workers than for state employees within the same job classifications, even after accounting for the costs of the benefits state employees receive.
- The contract workers at the three facilities possessed the necessary credentials to work within their classifications. However, they generally had an average of two to three years less tenure than state employees in the same job classifications, thus requiring the State to spend additional time and resources for training.
The Facilities Are Increasingly Using Contract Workers to Provide Health Care
The three facilities we reviewed overwhelmingly rely on state employees rather than contract workers to provide care. However, as they have struggled to fill vacant positions in recent years, they have increasingly needed to rely on contract workers to ensure adequate staffing. Hourly costs for contract workers are generally higher than for state employees in the same job classifications, although costs for some job classifications at Atascadero and Porterville have decreased recently. All three facilities have processes in place to ensure that contract workers have the licenses and qualifications necessary for their positions, but because the contract workers’ tenure at facilities tends to be shorter, they may have less familiarity with the needs of the population for whom they care.
The Facilities’ Use of Contract Workers
Contract workers made up a small share of overall staffing levels at each facility in fiscal year 2023–24, as Table 5 shows. For example, at Atascadero, contract workers accounted for 77 of the facility’s 1,513 authorized positions, or 5 percent; at Porterville, they accounted for 30 of the facility’s 763 authorized positions, or 4 percent; and at Salinas Valley, they accounted for 62 of the facility’s 637 authorized positions, or 10 percent.
Nevertheless, the number of hours worked by contract workers at each facility has increased dramatically over the years, as Figure 6 shows. We estimate that Porterville’s use of contract workers more than doubled from fiscal years 2019–20 to 2024–25, while Atascadero’s and Salinas Valley’s use of contract workers increased by 79 percent and 46 percent, respectively, during the same period.4 The majority of the contracted hours at each facility were in nursing classifications, as the figure illustrates. Specifically, the hours that contract workers covered in nursing classifications during fiscal years 2019–20 through 2024–25 constituted 87 percent of contract workers’ hours at Porterville, 60 percent of contract workers’ hours at Salinas Valley, and 57 percent of contract workers’ hours at Atascadero. After nursing classifications, the classifications in which contract workers covered the most hours varied by facility.
Figure 6
The Facilities’ Use of Contract Workers Has Increased Dramatically
Fiscal Years 2019–20 Through 2024–25

Source: Facilities’ contractor invoice data.
Note: Hours worked for fiscal year 2024–25 are projected based on data from July through December 2024.
* Salinas Valley hours worked do not include contract dental providers. Refer to further discussion in the Scope and Methodology in Appendix F.
Stacked column charts for the three facilities from 2019 to 2020 through 2024 to 2025 showing the increase in hours worked by contract staff by 79 percent at Atascadero, 172 percent at Porterville, and 46 percent at Salinas Valley overall across the groupings of Nursing, Mental Health, Psychiatry, Primary Care, and Other. Amounts are in the thousands of hours.
At Atascadero, in 2019 to 2020, contract staff worked over 31000 hours in the Nursing grouping, about 42000 hours in the Psychiatry grouping, just over 900 hours in the Primary Care grouping, and just over 6000 hours in the Other grouping. In 2020 to 2021, contract staff worked nearly 25000 hours in the Nursing grouping, about 45000 hours in the Psychiatry grouping, 0 hours in the Primary Care grouping, and just over 5200 hours in the Other grouping. In 2021 to 2022, contract staff worked just over 67000 hours in the Nursing grouping, nearly 43000 hours in the Psychiatry grouping, and nearly 4000 hours in the Other grouping. In 2022 to 2023, contract staff worked nearly 103000 hours in the Nursing grouping, over 1500 hours in the Mental Health grouping, over 43000 hours in the Psychiatry grouping, and nearly 17000 hours in the Other grouping. In 2023 to 2024, contract staff worked just over 105000 hours in the Nursing grouping, over 1000 hours in the Mental Health grouping, nearly 38000 hours in the Psychiatry grouping, and over 17000 hours in the Other grouping. In 2024 to 2025, contract staff worked just over 9000 hours in the Nursing grouping, just over 1000 hours in the Mental Health grouping, nearly 38000 hours in the Psychiatry grouping, 0 hours in the Primary Care grouping, and nearly 16000 hours in the Other grouping.
At Porterville, in 2019 to 2020, contract staff worked nearly 21000 hours in the Nursing grouping, 40 hours in the Mental Health grouping, nearly 40 hours in the Psychiatry grouping, over 800 hours in the Primary Care grouping, and over 8000 hours in the Other grouping. In 2020 to 2021 contract staff worked over 34000 hours in the Nursing grouping, nearly 16 hours in the Psychiatry grouping, nearly 1700 hours in the Primary Care grouping, and nearly 8800 hours in the Other grouping. In 2021 to 2022 contract staff worked just over 32000 hours in the Nursing grouping, over 80 hours in the Psychiatry grouping, 60 hours in the Primary Care grouping, and over 5300 hours in the Other grouping. In 2022 to 2023 contract staff worked over 53000 hours in the Nursing grouping, over 110 hours in the Mental Health grouping, over 170 hours in the Psychiatry grouping, nearly 70 hours in the Primary Care grouping, and over 6700 hours in the Other grouping. In 2023 to 2024 contract staff worked nearly 59000 hours in the Nursing grouping, over 200 hours in the Psychiatry grouping, nearly 70 hours in the Primary Care grouping, and over 5000 hours in the Other grouping. In 2024 to 2025 contract staff worked nearly 75000 hours in the Nursing grouping, 190 hours in the Psychiatry grouping, over 60 hours in the Primary Care grouping, and over 4500 hours in the Other grouping.
At Salinas Valley, in 2019 to 2020, contract staff worked over 46000 hours in the Nursing grouping, over 27000 hours in the Mental Health grouping, over 3700 hours in the Psychiatry grouping, over 1400 hours in the Primary Care grouping, and nearly 13000 hours in the Other grouping. In 2020 to 2021 contract staff worked over 63000 hours in the Nursing grouping, nearly 29000 hours in the Mental Health grouping, over 5700 hours in the Psychiatry grouping, nearly 4800 hours in the Primary Care grouping, and over 10400 hours in the Other grouping. In 2021 to 2022 contract staff worked over 64000 hours in the Nursing grouping, nearly 24000 hours in the Mental Health grouping, over 7000 hours in the Psychiatry grouping, over 5500 hours in the Primary Care grouping, and over 7000 hours in the Other grouping. In 2022 to 2023 contract staff worked nearly 78000 hours in the Nursing grouping, nearly 22000 hours in the Mental Health grouping, nearly 7000 hours in the Psychiatry grouping, over 6200 hours in the Primary Care grouping, and over 7200 hours in the Other grouping. In 2023 to 2024 contract staff worked over 84000 hours in the Nursing grouping, over 24000 hours in the Mental Health grouping, over 7100 hours in the Psychiatry grouping, nearly 2000 hours in the Primary Care grouping, and nearly 12000 hours in the Other grouping. In 2024 to 2025 contract staff worked nearly 83000 hours in the Nursing grouping, nearly 30000 hours in the Mental Health grouping, nearly 7000 hours in the Psychiatry grouping, over 2800 hours in the Primary Care grouping, and nearly 12000 hours in the Other grouping.
According to facility staff, the facilities increased their use of contract workers in part to fill their ongoing vacant positions. They explained that the facilities use contract workers to cover shifts when state employees are not available and that they increased their use of contract workers in part because they did not have enough state employees to work needed shifts. Staff also attributed the increase to the COVID‑19 pandemic, when each facility had to address pandemic‑related needs. For example, staff at Salinas Valley and Atascadero stated that they had to rely on contract staff to test patients for COVID‑19, treat patients who tested positive for the virus, and replace state employees who tested positive for COVID‑19 and had to isolate themselves. In addition, staff at Atascadero stated that a reduction in the number of mandatory overtime shifts and an increase in state employees being out on medical leave also led the facility to increase its use of contract workers.
The Number and Value of Health Care Contracts
As part of our review, the Joint Legislative Audit Committee (Audit Committee) asked us to determine the number and cost of each facility’s medical and mental health care staffing contracts. Each of the three facilities we audited takes a different approach to contracting for health care workers. Atascadero uses contracts that DSH enters into on the facility’s behalf, as well as contracts that the facility itself enters.5 Porterville executes its own staffing contracts with both staffing agencies and individual providers. CDCR maintains staffing contracts for Salinas Valley and other correctional facilities. It has had one contract in place for medical staffing since 2014 and a second contract with the same vendor since 2017—updated in 2022—for dental and mental health care staffing. We list the three facilities’ contracts in Appendix A.
The annual maximum value of the three facilities’ health care contracts increased by nearly two times to more than five times from fiscal years 2019–20 through 2024–25, although the facilities spent only a portion of the maximum contract values.6 Of the three facilities, Atascadero had the largest increase in the value of its contracts, from $65 million in fiscal year 2019–20 to $213 million in fiscal year 2024–25, as Figure 7 shows. The number of Atascadero’s contracts also more than doubled from 13 contracts to 28 contracts during this period.
Figure 7
The Projected Value of the Facilities’ Health Care Staffing Contracts and the Amounts the Facilities Spent on Contract Workers Have Generally Increased
Fiscal Years 2019–20 Through 2024–25

Source: Staffing contracts, contractor invoice data, and budget documents.
Note: Amount spent for fiscal year 2024–25 is projected based on data from July through December 2024. Salinas Valley contract amounts do not include contract dental providers. Refer to further discussion in the Scope and Methodology in Appendix F.
Stacked bar chart showing that from fiscal years 2019 to 2020 through 2024 to 2025, total projected value of health care staffing contracts increased at all three facilities, though total amount spent on these contracts was generally less than half of the total value of the contracts.
A callout box explains that each bar shows the projected value of the facility’s health care staffing contracts and the actual amount the facility spent on contract workers for that fiscal year.
During this time period, the total number of available contracts at Atascadero was 46, with a total projected contract value of 853112582 dollars. The total contract amount spent was 131719370 million dollars, 15 percent of the total maximum projected value. In fiscal year 2019 to 2020, the projected contract value was 65 million dollars, and the amount spent was 19 million dollars. In fiscal year 2020 to 2021, the projected contract value was 141 million dollars, and the amount spent was 19 million dollars. In fiscal year 2021 to 2022, the projected contract value was 147 million dollars, and the amount spent was 18 million dollars. In fiscal year 2022 to 2023, the projected contract value was 84 million dollars, and the amount spent was 28 million dollars. In fiscal year 2023 to 2024, the projected contract value was 203 million dollars, and the amount spent was 25 million dollars. In fiscal year 2024 to 2025, the projected contract value was 213 million dollars, and the amount spent was 22 million dollars.
During this time period, the total number of available contracts at Porterville was 101, with a total projected contract value of 60071699 dollars. 24146425 million dollars were spent on these contracts, 40 percent of the total projected value. In fiscal year 2019 to 2020, the projected contract value was 3 million dollars, and the amount spent was 3 million dollars. In fiscal year 2020 to 2021, the projected contract value was 14 million dollars, and the amount spent was 5 million dollars. In fiscal year 2021 to 2022, the projected contract value was 6 million dollars, and the amount spent was 3 million dollars. In fiscal year 2022 to 2023, the projected contract value was 5 million dollars, and the amount spent was 5 million dollars. In fiscal year 2023 to 2024, the projected contract value was 13 million dollars, and the amount spent was 4 million dollars. In fiscal year 2024 to 2025, the projected contract value was 18 million dollars, and the amount spent was 5 million dollars.
During this time period, the total number of available contracts at Salinas Valley was 3, with a total projected contract value of 154338940 dollars. 82697370 million dollars were spent on these contracts, 54 percent of the total projected value. In fiscal year 2019 to 2020, the projected contract value was 18 million dollars, and the amount spent was 9 million dollars. In fiscal year 2020 to 2021, the projected contract value was 25 million dollars, and the amount spent was 13 million dollars. In fiscal year 2021 to 2022, the projected contract value was 31 million dollars, and the amount spent was 13 million dollars. In fiscal year 2022 to 2023, the projected contract value was 17 million dollars, and the amount spent was 15 million dollars. In fiscal year 2023 to 2024, the projected contract value was 31 million dollars, and the amount spent was 16 million dollars. In fiscal year 2024 to 2025, the projected contract value was 32 million dollars, and the amount spent was 17 million dollars.
According to DSH’s former business management branch chief, the department projects contract values based on staffing needs in anticipation of a worst‑case scenario, such as another pandemic. She explained that the department now typically enters into contracts with multiple vendors for the same services to ensure that contract workers will be available when needed. She also stated that although the value of the contracts has increased, the facility pays for only the services it uses and does not spend or encumber the full value of the contracts. Further, Atascadero modified its contracting practices in 2023 to enter into contracts directly with vendors rather than using interagency agreements, increasing the number of its staffing contracts.
Although the number of Porterville’s health care staffing contracts remained fairly consistent from fiscal years 2019–20 to 2024–25, the annual value of those contracts increased five‑fold, from $3.5 million to $18 million. Porterville had a total of 101 staffing contracts with a total value of $60 million during this time. Porterville’s staff explained that before the pandemic, it used personal service contracts only for medical specialty services, such as neurology, cardiology, and ophthalmology. They stated that the facility now contracts with multiple vendors that provide contract workers in various health care job classifications and that its contracts with those vendors are larger than the specialty contracts it used in previous years.
Finally, the annual value of contracts that CDCR allotted to Salinas Valley almost doubled from $18.4 million in fiscal year 2019–20 to $32 million in fiscal year 2024–25. In each year during our review period, CDCR had one contract for medical staffing and another for dental and mental health care staffing, both with the same vendor. CDCR is able to maintain fewer contracts than the other facilities because its contracts are network contracts, in which the vendor subcontracts with other staffing agencies to provide contract workers. CDCR staff explained that increases in costs led to an increase in its contract values.
The Facilities’ Spending on Contract Workers
Although the three facilities did not spend all funds allocated to their staffing contracts during the years we reviewed, the annual amount each facility spent on contract workers has increased since fiscal year 2019–20. As Figure 8 shows, from fiscal years 2019–20 through 2024–25, we estimate that annual spending on contract staff increased by $3.3 million at Atascadero, by $1.7 million at Porterville, and by $7.6 million at Salinas Valley.
Figure 8
The Amount Each Facility Spent on Contract Workers Has Generally Increased
Fiscal Years 2019–20 Through 2024–25

Source: Facilities’ contractor invoice data.
Notes: Spending for fiscal year 2024–25 is projected based on data from July through December 2024.
Atascadero spent approximately $217,000 for primary care contract workers in fiscal year 2019–20, but did not use primary care contract workers for the rest of the audit period. Porterville spent $3,000 for mental health contract workers in fiscal year 2019–20 and $900 in fiscal year 2022–23, but did not use mental health contract workers in the other fiscal years during the audit period. Salinas Valley amounts do not include contract dental providers. Refer to further discussion in the Scope and Methodology in Appendix F.
Three line graphs show that from fiscal years 2019 to 2020 through 2024 to 2025, overall spending on contract workers has increased for all three facilities; 3.3. million dollars at Atascadero, 1.7 million dollars at Porterville, and 7.6 million dollars at Salinas Valley.
In fiscal year 2019 to 2020 at Atascadero, contract workers cost the facility 4.4 million dollars for nursing classifications, 500000 dollars for other classifications, 200000 dollars for primary care classifications, 14 million dollars for psychiatry classifications, and 19.1 million dollars overall. In fiscal year 2020 to 2021 at Atascadero, contract workers cost the facility 3.3 million dollars for nursing classifications, 400000 dollars for other classifications, 15.8 million dollars for psychiatry classifications, and 19.4 million dollars overall. In fiscal year 2021 to 2022 at Atascadero, contract workers cost the facility 2.7 million dollars for nursing classifications, 200000 for other classifications, 14.8 million dollars for psychiatry classifications, and 17.7 million dollars overall. In fiscal year 2022 to 2023 at Atascadero, contract workers cost the facility 200000 dollars for mental health classifications, 13.1 million dollars for nursing classifications, 1 million dollars for other classifications, 14 million dollars for psychiatry classifications, and 28.2 million dollars overall. In fiscal year 2023 to 2024 at Atascadero, contract workers cost the facility 100000 dollars for mental health classifications, 11.9 million dollars for nursing classifications, 1 million dollars for other classifications, 11.8 million dollars for psychiatry classifications, and 24.9 million dollars overall. In fiscal year 2024 to 2025 at Atascadero, contract workers cost the facility 100000 dollars for mental health classifications, 9.6 million dollars for nursing classifications, 900000 dollars for other classifications, 11.8 million dollars for psychiatry classifications, and 22.4 million dollars overall.
In fiscal year 2019 to 2020 at Porterville, contract workers cost the facility 3000 dollars for mental health classifications, 1.8 million dollars for nursing classifications, 900000 dollars for other classifications, 300000 dollars for primary care classifications, 5000 dollars for psychiatry classification, and 3 million dollars overall. In fiscal year 2020 to 2021 at Porterville, contract workers cost the facility 2.8 million dollars for nursing classifications, 1.1 million dollars for other classifications, 700000 dollars for primary care classifications, 3000 dollars for psychiatry classifications, and 4.5 million dollars overall. In fiscal year 2021 to 2022 at Porterville, contract workers cost the facility 2.7 million dollars for nursing classifications, 500000 dollars for other classifications, 9000 dollars for primary care classifications, 25000 dollars for psychiatry classifications, and 3.3 million dollars overall. In fiscal year 2022 to 2023 at Porterville, contract workers cost the facility 900 dollars for mental health classifications, 4 million dollars for nursing classifications, 600000 dollars for other classifications, 10000 dollars for primary care classifications, 50000 dollars for psychiatry classifications, and 4.6 million dollars overall. In fiscal year 2023 to 2024 at Porterville, contract workers cost the facility 3.1 million dollars for nursing classifications, 700000 dollars for other classifications, 13000 dollars for primary care classifications, 70000 dollars for psychiatry classifications, and 4 million dollars overall. In fiscal year 2024 to 2025 at Porterville, contract workers cost the facility 3.9 million dollars for nursing classifications, 700000 dollars for other classifications, 12000 dollars for primary care classifications, 60000 dollars for psychiatry classifications, and 4.7 million dollars overall.
In fiscal year 2019 to 2020 at Salinas Valley, contract workers cost the facility 3.6 million dollars for mental health classifications, 3 million dollars for nursing classifications, 700000 dollars for other classifications, 400000 dollars for primary care classifications, 1.5 million dollars for psychiatry classifications, and 9.2 million dollars overall. In fiscal year 2020 to 2021 at Salinas Valley, contract workers cost the facility 3.9 million dollars for mental health classifications, 4.8 million dollars for nursing classifications, 700000 dollars for other classifications, 1.3 million dollars for primary care classifications, 2.4 million dollars for psychiatry classifications, and 13.1 million dollars overall. In fiscal year 2021 to 2022 at Salinas Valley, contract workers cost the facility 3.4 million dollars for mental health classifications, 4.8 million dollars for nursing classifications, 500000 dollars for other classifications, 1.5 million dollars for primary care classifications, 2.8 million dollars for psychiatry classifications, and 13.1 million dollars overall. In fiscal year 2022 to 2023 at Salinas Valley, contract workers cost the facility 3.8 million dollars for mental health classifications, 6.1 million dollars for nursing classifications, 500000 dollars for other classifications, 1.7 million dollars for primary care classifications, 2.8 million dollars for psychiatry classifications, and 15 million dollars overall. In fiscal year 2023 to 2024 at Salinas Valley, contract workers cost the facility 4.4 million dollars for mental health classifications, 7 million dollars for nursing classifications, 700000 dollars for other classifications, 600000 dollars for primary care classifications, 2.8 million dollars for psychiatry classifications, and 15.5 million dollars overall. In fiscal year 2024 to 2025 at Salinas Valley, contract workers cost the facility 5.3 million dollars on mental health classifications, 7.1 million dollars on nursing classifications, 800000 dollars for other classifications, 900000 dollars for primary care classifications, 2.8 million dollars for psychiatry classifications, and 16.8 million dollars overall.
Most of this increased spending was due to the facilities’ growing use of contract workers in nursing classifications. From fiscal years 2019–20 through 2024–25, spending on contract nurses increased from $4.4 million to an estimated $9.6 million at Atascadero; from $1.8 million to an estimated $3.9 million at Porterville; and from $3 million to an estimated $7.1 million at Salinas Valley. Spending also increased in other classifications at each facility; for example, during our audit period, Salinas Valley increased its spending on contract mental health workers by about $1.6 million and on contract psychiatry by about $1.3 million. However, only Salinas Valley experienced increased spending in all five contract worker groupings. In fact, Atascadero’s and Porterville’s spending decreased in some categories, such as psychiatry and primary care. Nevertheless, Atascadero’s and Porterville’s increases in spending on nurses were significant enough to result in an overall increase in their spending on all contract workers, although Atascadero’s spending has declined somewhat since fiscal year 2022–23.
Hourly Costs for Contract Workers Are Generally Higher Than Those for State Employees
Our review of average hourly costs found that for most job classifications, the facilities incur higher hourly costs for contract workers than for their state counterparts, even after accounting for the State’s overhead and benefit costs.7 We list the overhead costs we included in our analysis in the text box. For example, as Table 6 shows, the three facilities incurred costs from $84 to $113 more per hour for contract psychiatrists in fiscal year 2024–25 than for state‑employed psychiatrists. For licensed vocational nurses, the per‑hour cost difference ranged from $5 to $19 that year. It is important to note that because Table 6 includes both the State’s overhead costs associated with the contracts and the State’s overhead costs for its employees, the per‑hour costs within it represent more than the actual wages that state employees or contract workers received.
Our Calculation of State Employee Hourly Costs Included the Following Elements:
- Gross pay
- Retirement system state share
- Social Security employer contribution
- Medicare employer contribution
- Other post-employment benefits employer contribution
- State disability insurance employer contribution
- State’s share of costs and contributions to benefits, such as health care, dental, and life insurance, among others.
Source: SCO data.
Facility staff offered several explanations for why they paid higher hourly rates for contract workers. Porterville stated that its persistent staffing challenges have led to vendor bid rates that are higher than what the facility pays state employees. Atascadero staff stated that competition with other departments, counties, and hospital systems had led to contract worker costs that are higher than state employee salaries. A procurement analyst at Salinas Valley asserted that the high cost of living in Monterey County contributed to difficulties recruiting contract workers for the facility, which led CDCR to increase contracting rates.
Although all three facilities generally pay more for contract workers than for state employees, Porterville’s and Atascadero’s hourly costs for some contract workers have actually decreased since fiscal year 2019–20, as Figure 9 shows. For example, the average hourly cost that Atascadero incurred for contract workers in nursing classifications declined from $136 in fiscal year 2019–20 to $105 in fiscal year 2024–25. Porterville’s average hourly cost for contract workers in nursing classifications similarly declined, from about $74 in fiscal year 2019–20 to about $55 in fiscal year 2024–25. Because the majority of the contract workers at these facilities worked in nursing classifications during our review period, the facilities’ overall average hourly costs also declined, by 34 percent at Atascadero and 35 percent at Porterville.
Figure 9
Average Hourly Costs for Contract Workers in Some Job Classification Groups at Atascadero and Porterville Have Declined
Fiscal Year 2019–20 Through Fiscal Year 2024–25
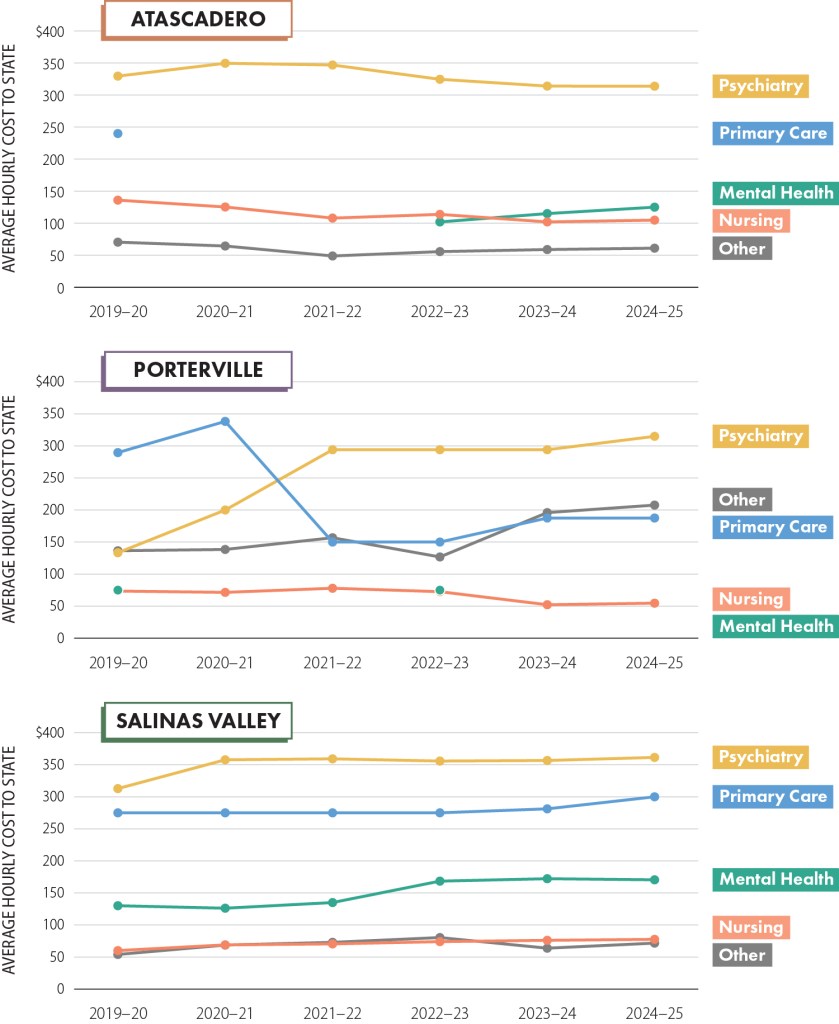
Source: Facility invoice data.
Notes: Data for fiscal year 2024–25 is projected based on data from July through December 2024.
Atascadero paid $240 per hour on average for primary care contract workers in fiscal year 2019–20, but did not use primary care contract workers for the rest of the audit period. Porterville paid $75 per hour on average for mental health contract workers in fiscal year 2019–2020 and fiscal year 2022–23, but did not use mental health contract workers in the other fiscal years during the audit period. Salinas Valley figures do not include contract dental providers. See further discussion in the Scope and Methodology section.
Three line graphs show that from fiscal years 2019 to 2020 through 2024 to 25, the average hourly cost to State for some classifications of health care contract workers have decreased at Atascadero and Porterville, while all classifications at Salinas Valley have increased in cost per hour in our groupings.
At Atascadero, in fiscal year 2019 to 2020 at Atascadero, the average cost per hour for contract workers was 136 dollars for nursing classifications, 70 dollars for other classifications, 240 dollars for primary care classifications, and 329 dollars for psychiatry classifications. In fiscal year 2020 to 2021 at Atascadero, the average cost per hour for contract workers was 125 dollars for nursing classifications, 64 dollars for other classifications, and 350 dollars for psychiatry classifications. In fiscal year 2021 to 2022 at Atascadero, the average cost per hour for contract workers was 108 dollars for nursing classifications, 49 dollars for other classifications, and 347 dollars for psychiatry classifications. In fiscal year 2022 to 2023 at Atascadero, the average cost per hour for contract workers was 102 dollars for mental health classifications, 114 dollars for nursing classifications, 56 dollars for other classifications, and 325 dollars for psychiatry classifications. In fiscal year 2023 to 2024 at Atascadero, the average cost per hour for contract workers was 115 dollars for mental health classifications, 102 dollars for nursing classifications, 59 dollars for other classifications, and 314 dollars for psychiatry classifications. In fiscal year 2024 to 2025 at Atascadero, the average cost per hour for contract workers was 125 dollars for mental health classifications, 105 dollars for nursing classifications, 61 dollars for other classifications, and 314 dollars for psychiatry classifications.
At Porterville, in fiscal year 2019 to 2020, the average cost per hour for contract workers was 75 dollars for mental health classifications, 73 dollars for nursing classifications, 136 dollars for other classifications, 291 dollars for primary care classifications, and 133 dollars for psychiatry classifications. In fiscal year 2020 to 2021 at Porterville, the average cost per hour for contract workers was 72 dollars for nursing classifications, 138 dollars for other classifications, 341 dollars for primary care classifications, and 200 dollars for psychiatry classifications. In fiscal year 2021 to 2022 at Porterville, the average cost per hour for contract workers was 78 dollars for nursing classifications, 157 dollars for other classifications, 150 dollars for primary care classifications, and 294 dollars for psychiatry classifications. In fiscal year 2022 to 2023 at Porterville, the average cost per hour for contract workers was 75 dollars for mental health classifications, 73 dollars for nursing classifications, 127 dollars for other classifications, 150 dollars for primary care classifications, and 294 dollars for psychiatry classifications. In fiscal year 2023 to 2024 at Porterville, the average cost per hour for contract workers was 52 dollars for nursing classifications, 196 dollars for other classifications, 188 dollars for primary care classifications, and 294 dollars for psychiatry classifications. In fiscal year 2024 to 2025 at Porterville, the average cost per hour for contract workers was 55 dollars for nursing classifications, 208 dollars for other classifications, 188 dollars for primary care classifications, and 315 dollars for psychiatry classifications.
At Salinas Valley, in fiscal year 2019 to 2020, the average cost per hour for contract workers was 130 dollars for mental health classifications, 60 dollars for nursing classifications, 54 dollars for other classifications, 275 dollars for primary care classifications, and 313 dollars for psychiatry classifications. In fiscal year 2020 to 2021 at Salinas Valley, the average cost per hour for contract workers was 126 dollars for mental health classifications, 69 dollars for nursing classifications, 69 dollars for other classifications, 275 dollars for primary care classifications, and 358 dollars for psychiatry classifications. In fiscal year 2021 to 2022 at Salinas Valley, the average cost per hour for contract workers was 135 dollars for mental health classifications, 70 dollars for nursing classifications, 73 dollars for other classifications, 275 dollars for primary care classifications, and 359 dollars for psychiatry classifications. In fiscal year 2022 to 2023 at Salinas Valley, the average cost per hour for contract workers was 168 dollars for mental health classifications, 74 dollars for nursing classifications, 80 dollars for other classifications, 275 dollars for primary care classifications, and 356 dollars for psychiatry classifications. In fiscal year 2023 to 2024 at Salinas Valley, the average cost per hour for contract workers was 172 dollars for mental health classifications, 76 dollars for nursing classifications, 64 dollars for other classifications, 281 dollars for primary care classifications, and 357 dollars for psychiatry classifications. In fiscal year 2024 to 2025 at Salinas Valley, the average cost per hour for contract workers was 170 dollars for mental health classifications, 78 dollars for nursing classifications, 72 dollars for other classifications, 300 dollars for primary care classifications, and 361 dollars for psychiatry classifications.
Staff at Atascadero and Porterville cited the end of the COVID‑19 pandemic and their ability to use the contract bidding process to select the lowest responsible bidder as reasons that they were able to obtain lower rates. Using the contract bidding process, Atascadero and Porterville were able to obtain new contracts with lower rates, as the text box shows. Staff from both facilities stated that previous contracts were executed as emergency contracts and did not go through the bidding process. According to Atascadero, it began to use DSH’s statewide multifacility contracts during our audit period, which also resulted in lower hourly costs for contract workers. As a result of their lower hourly costs, Atascadero’s and Porterville’s increased spending on contract workers during our review period, which Figure 10 shows, was less than it otherwise would have been.
Contract Rates for Some Classifications at Atascadero and Porterville Were Lower in 2024 Than in 2020
| Contract Rates* | ||
|---|---|---|
| 2020 | 2024 | |
| Atascadero | ||
| • Licensed Vocational Nurses • Registered Nurses | $76 126 | $55 113 |
| Porterville | ||
| • Certified Nursing Assistants • Psychiatric Technicians • Licensed Vocational Nurses • Registered Nurses | $55 75 75 95 | $49 65 66 89 |
Source: Facility contracts.
* Contract rates include administrative overhead charges. Values shown are examples from specific contracts and may differ from the averages we show in Table 6.
Figure 10
Hours Worked and Total Cost of Contract Workers at Each Facility Have Increased
Fiscal Year 2019–20 Through Fiscal Year 2024–25

Source: Facility invoice data.
Notes: Spending and hours worked for fiscal year 2024–25 are projected based on data from July through December 2024.
* Salinas Valley figures do not include contract dental providers. See further discussion in the Scope and Methodology section.
Three clustered column charts show the total hours worked and total costs incurred for contract workers at the three facilities for fiscal years 2019 to 2020 through 2024 to 2025.
In fiscal year 2019 to 2020, contract health care workers at Atascadero worked 81000 hours and cost the facility 19 million dollars. In fiscal year 2020 to 2021, contract health care workers at Atascadero worked 75000 hours and cost the facility 19 million dollars. In fiscal year 2021 to 2022, contract health care workers at Atascadero worked 71000 hours and cost the facility 18 million dollars. In fiscal year 2022 to 2023, contract health care workers at Atascadero worked 156000 hours and cost the facility 19 million dollars. In fiscal year 2023 to 2024, contract health care workers at Atascadero worked 161000 hours and cost the facility 25 million dollars. In fiscal year 2024 to 2025, contract health care workers at Atascadero worked 144000 hours and cost the facility 22 million dollars.
In fiscal year 2019 to 2020, contract health care workers at Porterville worked 29000 hours and cost the facility 3 million dollars. In fiscal year 2020 to 2021, contract health care workers at Porterville worked 45000 hours and cost the facility 5 million dollars. In fiscal year 2021 to 2022, contract health care workers at Porterville worked 38000 hours and cost the facility 3 million dollars. In fiscal year 2022 to 2023, contract health care workers at Porterville worked 60000 hours and cost the facility 5 million dollars. In fiscal year 2023 to 2024, contract health care workers at Porterville worked 64000 hours and cost the facility 4 million dollars. In fiscal year 2024 to 2025, contract health care workers at Porterville worked 80000 hours and cost the facility around 5 million dollars.
In fiscal year 2019 to 2020, contract health care workers at Salinas Valley worked 92000 hours and cost the facility around 9 million dollars. In fiscal year 2020 to 2021, contract health care workers at Salinas Valley worked 113000 hours and cost the facility 13 million dollars. In fiscal year 2021 to 2022, contract health care workers at Salinas Valley worked 108000 hours and cost the facility 13 million dollars. In fiscal year 2022 to 2023, contract health care workers at Salinas Valley worked 120000 hours and cost the facility 15 million dollars. In fiscal year 2023 to 2024, contract health care workers at Salinas Valley worked 129000 hours and cost the facility 16 million dollars. In fiscal year 2024 to 2025, contract health care workers at Salinas Valley worked 134000 hours and cost the facility 17 million dollars.
Atascadero and Porterville also controlled the growth in their overall contracting costs by limiting their use of registered nurses, who have the highest hourly costs among the nursing classifications. In fiscal year 2019–20, registered nurses accounted for 100 percent of the total hours worked by contract nurses at Atascadero and 34 percent of the hours worked by contract nurses at Porterville. In contrast, by fiscal year 2024–25, registered nurses made up 74 percent of the hours worked by contract nurses at Atascadero and just 14 percent of the hours worked by contract nurses at Porterville. At each facility, contract nurses in classifications with lower hourly rates made up the difference. Consequently, the hourly cost for the overall nursing grouping at these two facilities decreased during our review period.
Unlike at Porterville and Atascadero, average hourly costs for contract workers at Salinas Valley generally increased in all categories from fiscal years 2019–20 through 2024–25, as Figure 9 shows. The average hourly rates that Salinas Valley paid for all contract health care workers increased by 25 percent over this period. According to facility staff, the staffing contract CDCR uses for all its facilities includes additional funds for its vendor to offer contract workers higher wages as a recruiting tool. In addition, Salinas Valley used proportionally more contract registered nurses in fiscal year 2024–25 than in fiscal year 2019–20. In fiscal year 2019–20, registered nurses accounted for 13 percent of Salinas Valley’s contract worker hours in the nursing grouping; by fiscal year 2024–25, this number had increased to 24 percent.
The Three Facilities Generally Ensure That Contract Workers Are Qualified for Their Positions
The three facilities we reviewed require that contract workers have the same licenses and certificates (credentials) and meet the same or higher qualifications as those that the State requires for state employees in the same classifications. For example, the three facilities hire contract workers for a variety of positions that require special credentials, including licensed vocational nurse, psychiatric technician, registered nurse, and certified nursing assistant. The facilities generally specify these credential requirements in their staffing contracts with vendors. To determine whether contract workers possessed necessary credentials at the time of starting work and throughout their tenure with the three facilities, we reviewed documentation from 30 contract workers at each of the facilities. We found that all of the contract workers we reviewed maintained valid and appropriate credentials throughout their contract assignment, as Table 7 shows.
The three facilities require their contractors to verify that all contract workers possess the required credentials. The three facilities told us that they also independently verify or review credential documentation and track credential expiration dates for at least some contract workers. Specifically, Salinas Valley staff told us that they verify and track all contract worker licenses. Atascadero staff stated that they verify licenses and track expiration dates for nursing positions. Porterville staff explained that they verify and track this information for specialty contract workers but rely on the staffing agencies to do so for other positions.
The Short Tenure of Contract Workers Can Create Challenges for the Three Facilities
In part because the facilities generally use contract workers on a temporary basis, they had significantly shorter average tenures than state employees during our audit period. This shorter tenure can create challenges for the facilities because they must devote time and resources to training individuals who may only work for a short time. In addition, some state employees we interviewed explained that contract workers are not always familiar with the specific needs of the populations they serve.
Contract Workers’ Length of Tenure
Our review found that contract workers generally had significantly shorter average tenures than state employees at all three facilities.8 Specifically, except for psychiatry at Atascadero, contract workers in all groupings across all facilities had an average tenure of less than one year from July 2019 through December 2024, as Table 8 shows. In contrast, the average tenure during our audit period of state employees in the classification groupings we reviewed ranged from 1.7 years for psychiatrists at Salinas Valley to about 4.4 years for the primary care grouping at Atascadero. Across all groupings, the average tenure of state employees at Salinas Valley was almost 2 years longer than the tenure of contract workers, while the average tenures of state employees at Atascadero and Porterville ranged from almost 2.5 years to more than 3 years longer, respectively, than that of contract workers. We also measured the tenure for these state employees including their time at the facilities before July 2019, and found that many worked at the facilities for a significant amount of time. For example, the average state employee tenure for all groupings at Atascadero was more than 8.5 years, with psychiatrists averaging nearly 12 years. Although we did not attempt to measure the tenure of contract workers prior to our audit period, given their short tenure during our review period, and the fact that facilities generally use contract workers on a temporary basis, it is unlikely that the contract workers who worked during our audit period had significant tenure at the facilities before July 2019.
The short tenure of contract workers is due, in part, to the fact that the facilities generally use contract workers to meet temporary rather than long‑term needs. As we describe in the Introduction, personal service contracts are permissible under several conditions, including when the services are temporary in nature. One of the reasons the facilities we reviewed used to justify their contracts was that the services for which they contracted were temporary. In alignment with this justification, Porterville’s nursing coordinator stated that the facility typically signs contract workers to agreements that are, on average, three to six months in length because contract work is intended to be short‑term. Therefore, it is reasonable that many contract workers who worked during our audit period had an average tenure of less than one year.
Facility staff provided additional explanations for why the tenure of contract workers at their facilities is generally short‑term. For example, staff at DSH asserted that some contract staff relocate to the Atascadero area on a temporary basis but never intend to stay long term. However, DSH staff also asserted that psychiatrists sometimes have the financial flexibility to stay in the Atascadero area longer, which may explain why contract psychiatrists have higher tenure than other contract staff at the facility. Each facility’s staff also acknowledged that the secure detention settings often surprise contract staff and may discourage them from staying at the facility for longer periods of time.
Challenges Arising From the Use of Contract Workers
The short tenure of contract workers—who often stay in their positions at a facility for less than one year—can create challenges for facilities that need to provide training and instruction to these workers to enable them to complete their assignments. A 2017 study on nursing turnover found that one of the largest categories of costs related to turnover is orientating and training new hires.9 Further, a 2024 article on nursing challenges published by the U.S. Department of Health and Human Services suggests that to provide high‑quality care, contract health care nurses may need to spend time preparing for assignments.10 However, staff at all three facilities we reviewed stated that the facilities do not always have time to provide contract workers with all training and orientation necessary before they must start work.
Each facility provides an onboarding process for contract workers before those workers begin interacting with patients. According to the human resources director at Atascadero, contract workers receive the same two‑week orientation the facility provides to state employees. DSH staff indicated that the new employee orientation training is offered on a regular basis, and the department does not perceive this training as a significant challenge. Porterville similarly provides a new‑employee orientation to its contract workers, and it also expects each of its supervisors to provide contract workers with information about the facility and training related to their assignments. Salinas Valley provides a two‑week orientation to contract workers—one week of structured training followed by a one‑week clinical orientation. However, this orientation is shorter than the eight‑ to nine‑week training that state employees receive.
Nonetheless, when facilities use contract workers who are unfamiliar with a facility to perform the work of experienced long‑term state employees, it places an additional burden on state employees who must provide on‑the‑job training to contract workers while also providing care to patients. State employees at all three facilities described needing to interrupt their work to help contract workers complete tasks and assignments. Some state employees asserted that some contract workers are not always sufficiently trained or not trained specifically for the unit to which they are assigned, limiting their ability to perform their duties independently. Staff gave us examples of needing to show contract workers where to access medication and supplies because of their lack of familiarity with a unit. Other staff described situations when contract workers felt unprepared for the role and requested more training.
In addition, when facilities experience high contract worker turnover, it can disrupt the continuity of patient care and put the quality of that care at risk. Our review did not specifically look for quality‑of‑care lapses related to the use of contract workers, and we did not incidentally identify any such lapses at the three facilities we reviewed. Moreover, according to the 2024 article from the U.S. Department of Health and Human Services on nursing challenges we previously mentioned, the practice of using contract workers itself is not an indicator of unsafe patient care. However, the article stated that the inclusion of other factors such as staffing levels, staff experience levels, and work environment, can contribute to conditions that may be less safe for patients. We list some of the potential negative impacts high nursing turnover can have on patient care in the text box. The article also reports that a strong work environment characterized by adequate nurse support provides safety benefits to patients, and it suggests that care settings with a high use of contract nurses tend to have less strong work environments.
High Staffing Turnover Can Affect Quality of Care in a Number of Ways
- Discontinuity of care
- Missed nursing care
- Negative patient outcomes
- Incomplete patient information in handoffs
- Competing priorities between patients
Source: Auditor review of research, facility documentation, and interviews with facility staff.
Further, the facilities’ contract workers may not always be equipped to provide necessary care in difficult situations because they lack experience with the patients the facilities serve. In many health care settings, patients receive care for a few days or weeks before leaving. However, most of the individuals at the three facilities we reviewed require regular or even constant care for an extended period of time. Facility staff described how their familiarity with patients can help prevent unwanted patient outcomes, such as suicides, because they notice warning signs and provide interventions.
Finally, some state employees we interviewed expressed that they have at times lost confidence in contract workers who appeared unable to handle the high‑stress environment, leading the state employees to address patient needs alone. These employees explained that contract workers’ unfamiliarity with facility policies makes them less likely to know how to respond when a patient exhibits behavior that requires immediate intervention. Nevertheless, our interviews and review of a selection of shift‑staffing reports at Salinas Valley and Porterville found that the facilities assigned both state employees and contract workers to suicide watches and other one‑on‑one watches of at‑risk patients. Although using a contract worker is preferable to having insufficient staffing, relying on staff who may not be familiar with the facility or the specific needs of its population may increase the risk of poorer quality of care in such instances.
CDCR, DDS, and DSH Have Not Taken Necessary Steps to Ensure That Their Facilities Have Appropriate Staffing Levels
Key Points
- DDS and DSH lack policies and procedures for aligning their facilities’ budgeted medical and mental health care positions with the facilities’ operational needs. In the absence of such policies and procedures, they cannot ensure that their budgeted positions for medical and mental health care staff are sufficient to cover legally required staff‑to‑patient ratios.
- From fiscal years 2019–20 through 2024–25, each of the departments we reviewed had significant savings resulting from vacant medical and mental health care positions. However, the departments do not track vacancy savings at the position level, nor does the State require them to do so. As a result, we could not identify how they used the funding from the vacant positions we reviewed.
- None of the departments require their facilities to track and report instances when they do not meet required shift‑staffing minimums, leaving the departments without sufficient information to conduct appropriate oversight of the provision of medical and mental health care.
Two of the Three Departments Were Unable to Justify How They Budget for Health Care Staff
The State Administrative Manual (SAM) describes the process state agencies must use to reconcile staff positions during the annual state budgeting process, as well as to request changes to legislatively approved positions throughout the year. According to the SAM, agencies should base their estimates of expenditures and revenue on existing law and policies. In doing so, they must coordinate with the Department of Finance (Finance), which reviews their annual budgets and budget change proposals, including the number of authorized positions.
Finance expects all state departments to have proper fiscal internal controls for budgeting and accounting, including a system of policies and procedures for compliance with applicable laws, criteria, standards, and other requirements. However, we found that neither DSH nor DDS has such systems of policies and procedures to demonstrate proper fiscal internal controls for their staff budgeting processes. Both departments generally agreed that comprehensive policies and procedures for budgeting, including evaluating their departments’ number of authorized positions, is a necessary internal control. However, neither could tell us why they have not developed such policies and procedures.
CDCR has a high‑level, one‑page policy and procedure requiring its staff to evaluate staffing needs twice annually using staffing models that consider statutory and regulatory requirements for health care staff‑to‑patient ratios, as Table 9 shows. CDCR also has comprehensive staffing models that it based on legal and regulatory staffing minimums that it uses to ensure that it budgets medical and mental health positions according to its needs each year. For example, the nursing staffing model calculates the staffing necessary to achieve 3.5 nursing hours per patient per day in basic and skilled nursing care and 4.5 nursing hours per patient per day in intermediate care—both of which achieve the State’s minimum staffing requirements. CDCR was able to demonstrate that it used these staffing models to evaluate its staffing needs for budget projections twice annually. As a result, CDCR could demonstrate that it budgets facility positions based on required levels of care.
Without policies and procedures for developing budgets, DDS could not justify that its authorized positions for medical and mental health care staff were sufficient or necessary. DDS has a staffing model that staff stated they use to budget medical and mental health positions for Porterville; however, DDS has not updated this model since 2016 despite significant operational changes at Porterville, including closing its general treatment area in fiscal year 2019–20. Further, the staffing model does not demonstrate that DDS considers the number of staff needed to cover all positions and shifts based on the staff‑to‑patient ratios that state regulations require. DDS also could not demonstrate that it consistently used its staffing model or conducted any other evaluation of staffing needs each year. DDS’s fiscal forecasting branch manager explained that DDS uses its staffing model when it requests new resources. He further explained that DDS does not request additional funding for positions at facilities until its overall program, including all of its facilities, demonstrates a need. The branch manager’s explanation suggests that DDS only needs to perform a staffing analysis when the program requires additional staff. However, we believe an annual evaluation of staffing needs would also identify when positions may no longer be necessary because of operational changes.
DSH also could not justify that its staffing level was sufficient or necessary because it does not review its staffing needs for all medical and mental health positions annually. DSH developed a staffing model in 2019 that it still uses, and used it to support two legislatively‑approved budget requests for additional resources during our audit period. DSH’s chief financial officer stated that it uses this staffing model to assess staffing needs when there is a significant change in the number of patients the facility can care for, based on changes in the treatment that patients need or when it activates or closes a unit within the facility. DSH’s director explained that the department could use the staffing model to evaluate all medical and mental health care staffing needs annually, but acknowledged that the department has not done so previously. Budgeting staff positions consistently and appropriately is critical to ensuring that the departments can ask the Legislature to approve the positions necessary for facilities to meet their operational needs, while not having unnecessary positions that may remain vacant for extended periods of time.
The State Does Not Require the Three Departments to Track Facility Vacancy Savings at the Position Level
The Audit Committee asked us to identify how each department handled any funding budgeted for mental health care but not spent because of staff vacancies—funding that the State refers to as vacancy savings. During our audit period, all three facilities and their respective departments realized significant vacancy savings from unfilled medical and mental health care positions. However, we did not identify state law requiring the departments to track their use of vacancy savings at the position level, which would be necessary for us to determine vacancy savings specifically related to unfilled medical and mental health care positions.
Even after accounting for State employees’ overtime and contract workers’ hours, each facility we reviewed still had a significant number of uncovered vacant positions throughout our audit period, as Table 10 shows, which draws into question why the facilities need these additional positions. According to CDCR’s deputy director of fiscal management in its health care services division, CDCR staffs its facility in accordance with its court‑ordered staffing plan, leaving it little flexibility to reduce its position authority. Because DDS’s staffing plan is outdated, the assistant deputy director of its state‑operated facilities division acknowledged that it may be budgeting unnecessary positions. He said DDS is currently updating its staffing plan and working with Finance to align its authorized positions with its needs. When we asked Atascadero whether it needed its approximately 100 to more than 200 vacant positions, the executive director asserted that the facility needs all the allocated positions so the facility can provide the best possible care and can have staffing flexibility should it need to open a unit on short notice to accommodate new patients. Further, Atascadero’s assistant clinical administrator stated that the facility needs about 100 positions in the event it needs to open its three units that are currently closed. Although we recognize Atascadero’s need for flexibility and its desire to provide better care than the minimum required, the significant number of vacant positions raises questions as to whether maintaining all those positions is necessary, and because DSH does not annually use its staffing model to evaluate its needs, it lacks the evidence to support its position.
As a result of these vacancies, each facility we reviewed accumulated significant vacancy savings over the six fiscal years of our audit period: $247 million for Atascadero, $188 million for Salinas Valley, and about $157 million for Porterville, as Table 11 shows. These vacancy savings represented from 30 percent to 47 percent of the three facilities’ budgets for medical and mental health care positions during this period. Funding for vacant nursing positions alone accounted for 81 percent of Porterville’s cumulative vacancy savings, 69 percent of Atascadero’s cumulative savings, and 52 percent of Salinas Valley’s cumulative vacancy savings from fiscal years 2019–20 through 2024–25. Moreover, these estimates do not include the facilities’ savings related to benefits, overtime, and paid leave.
Agencies may use their funds in any manner consistent with the purposes for which the funds were appropriated by the Legislature and in accordance with their departmental budgets as approved by the Department of Finance. The annual state budget act also allows Finance to approve transfers within individual items of appropriation under certain circumstances. Accordingly, vacancy savings in one area may generally be used to cover shortfalls in another area.
For example, the state budget for fiscal year 2025–26 appropriated about $4.1 billion dollars to CDCR to support the department, of which about $2.7 billion dollars were scheduled for adult medical services and about $729 million were scheduled for adult mental health services. Because the appropriation is not specific to an individual facility, using medical services‑related savings at one of its facilities to cover a shortfall at another facility would be consistent with the appropriation, provided that the funds are used to pay for medical services. CDCR could also potentially use vacancy savings from medical services for mental health service shortfalls, within and across facilities. However, this would require CDCR to submit a formal request to Finance that outlines the amount of funds that the department intends to move and the underlying reasons for moving the funds.
According to their budgeting staff, none of the three departments track vacancy savings at the individual position or classification level. As a result, the departments could not explain how they used the facilities’ vacancy savings specific to the positions we reviewed. However, the budget staff asserted that their departments generally used vacancy savings to offset the costs associated with staff overtime and contract workers, as well as to pay for expenses such as equipment and special repairs. For example, staff indicated that in fiscal year 2020–21 DSH approved Atascadero’s emergency request for about $13,000 to replace a sewage pump for its water treatment facility.
Although the departments could not explain how they used the specific savings that we identified, they have reverted unused funds to the State in the past. Generally, unspent appropriated funds revert back to the State after a period of time, and each of the three departments asserted that they reverted funds to the General Fund during our review period. Specifically, budget staff from CDCR stated that it reverted about $16.4 million in salary savings from the fiscal year 2019–20 appropriation for its Mental Health Program back to the State; however, they acknowledged that there have been no similar reversions since. DDS also reverted $36 million of its fiscal year 2019–20 appropriation for its Residential and Community Services Program back to the General Fund at the end of fiscal year 2021–22. Similarly, DSH reverted about $1.4 million to the General Fund in fiscal year 2021–22 because of construction delays and COVID-19-related uncertainties. However, because these appropriations are made at the program-level, the departments could not determine whether the related reverted amounts included any vacancy savings from the specific positions that we reviewed.
The Departments Do Not Have a Formal Process for the Facilities We Reviewed to Report Whether They Are Meeting Staffing Requirements
State regulations establish specific staffing requirements per shift with which the three facilities we reviewed must comply. However, none of the facilities formally track this information, and their respective departments do not require them to report when they fail to meet shift‑staffing minimums. In addition, the federal court ordered CDCR to fill 90 percent or more of certain authorized medical and mental health care positions. However, as we previously discussed, it has consistently failed to comply with this order.
Shift‑Staffing Minimums
State regulations set forth minimum shift‑staffing requirements for facilities that differ by facility licensure type, as the text box shows. However, neither Porterville nor Salinas Valley has a formal process to track, tabulate, or report to their departments when they fail to meet these staffing minimums. Porterville and Salinas Valley track some shift‑staffing information, but their tracking mechanisms lack key components, such as the type of treatment to be delivered or the number of patients per shift to demonstrate that the staff who are scheduled and present are sufficient to meet the required staff‑to‑patient ratios. In contrast, Atascadero has a written process to schedule and track staffing to ensure that it meets the minimum staffing requirements and notifies its department when it does not. Although Atascadero does not tabulate the number of times it misses staffing minimums, according to its executive director, he notified the department of three shifts wherein the facility missed staffing minimums within our audit period. Staff at each facility asserted that they generally use state employee overtime, contract workers, or staff from other units to cover shift vacancies and that they rarely fall short of required staffing minimums. However, without a formal process to track, tabulate, and report such information to their respective departments, none of the facilities could demonstrate their full compliance with associated state or court requirements.
Examples of Regulatory Requirements for Shift Staffing
Acute Psychiatric Hospital—Must provide a sufficient number of appropriate personnel, which the regulation does not define.
Correctional Treatment Center—Must provide 2.5 nursing hours per patient day.
General Acute Care Hospital—Must provide the following:
- One nurse for every two patients in critical care.
- One nurse for every five patients in medical and surgical care.
- One nurse for every four patients in specialty care.
Intermediate Care Facility—Must provide a minimum average of 1.1 nursing hours per patient day.
Source: State regulations.
None of the departments responsible for overseeing the three facilities has formally or specifically requested that facilities track, tabulate, and report their compliance with staffing minimums or developed a formal process for the facilities to do so. Without such oversight, the departments cannot be certain that their facilities are staffed appropriately for each shift to provide adequate medical and mental health care. In fact, as we discuss in the Introduction, a 1981 court order required DSH and DDS to meet certain staffing minimums for nursing care, post the minimum staffing requirements for each shift, tabulate the number of people by which each shift fell short, and aggregate this information in a quarterly report to headquarters. Although the departments no longer follow the court order and it is likely no longer enforceable, the requirements serve as a best practice for accountability, transparency, and effective oversight of facilities’ medical and mental health staffing.
The departments provided various explanations for not requiring facilities to track, tabulate, and report staffing minimums. DSH’s chief deputy director of operations (chief deputy) acknowledged that DSH lacks such a formal process but stated that it generally expects that its facilities will report staffing shortages to DSH. Atascadero’s executive director also confirmed that there is no formalized process that requires such reporting. Similarly, the assistant chief counsel for DDS advised that the department has an unwritten expectation that its facilities will report to the department any time that a staffing issue prevents them from meeting the minimum staffing requirements in state regulations. However, DDS was also unable to demonstrate how it monitors Porterville’s shift staffing. Both DDS and DSH generally agreed that tracking such information would be beneficial.
Finally, according to CDCR’s former deputy director of business services for CCHCS (business services deputy), CDCR similarly does not require Salinas Valley to track, tabulate, and report shift‑staffing shortages for medical and mental health care units. She stated that the facility’s chief executive officer of health care is responsible for oversight, management, and compliance related to shift‑staffing minimums. CDCR’s director of health care policy and administration acknowledged the need to ensure that its licensed facilities meet shift‑staffing requirements. As a result, she explained that CDCR is currently formalizing a process for facilities to track, tabulate, and report any staffing deficiencies to the department.
Position‑Staffing Minimums
As the Introduction explains, in addition to being subject to regulatory shift‑staffing requirements for its licensed facilities, CDCR is subject to additional position‑staffing requirements at the direction of the federal court. Specifically, the court has directed CDCR to fill certain mental health care positions, such as psychiatrists, psychologists, and clinical social workers, at 90 percent or greater, and to report its vacancy rates for these positions to the court each month. Additionally, the federal receiver’s staffing plan indicates that CDCR has established the same goal for its medical positions, including nurses.
Nevertheless, when we reviewed CDCR’s monthly reports for these and other medical and mental health positions from fiscal years 2019–20 through 2024–25, we found that Salinas Valley met the court’s requirements and its own goals for just 31 percent to 55 percent of the positions it reported annually, as Figure 11 shows. The facility appeared to have the most difficulty filling mental health positions: it filled psychology positions at the required level only 23 percent of the time, clinical social workers 17 percent of the time, and other mental health positions 33 percent of the time. Salinas Valley most closely met its position‑staffing requirements for the primary care and psychiatry job classification groups, but it still reported that it filled each of those positions at the required level only 49 percent of the time.
Figure 11
Salinas Valley Met Its Position‑Staffing Requirements Less Than Half of the Time From
Fiscal Years 2019–20 Through 2024–25

Source: CDCR’s monthly vacancy reports.
Column chart shows percentage of positions filled at the required level from fiscal years 2019 to 2020 through 2024 to 2025 at Salinas Valley. In 2019 to 2020, the facility was at 44 percent of positions filled at the required level. In 2020 to 2021, the facility was at 55 percent of positions filled at the required level. In 2021 to 2022 and 2022 to 2023, the facility was at 35 percent of positions filled at the required level. In 2023 to 2024, the facility was at 31 percent of positions filled at the required level. In 2024 to 2025 the facility was at 40 percent of positions filled at the required level.
Other Areas We Reviewed
To address the audit objectives approved by the Audit Committee, we also did the following:
- Reviewed shift‑staffing reports from the three facilities to determine staffing trends. We found that state employees, rather than contract workers, provided the majority of patient care.
- Conducted interviews with state employees and contract workers to gain insight into the perspectives of frontline workers.
State Employees Generally Provided the Majority of Patient Care Across Shifts at the Three Facilities
The Audit Committee asked us to determine the provision of patient care and the number of patients seen by state employees and contract workers. To accomplish this, we reviewed staffing reports for 126 shifts at each facility for the same seven‑day period each year from 2019 through 2024 to determine the composition of the facility’s shift‑staffing. Further, because Atascadero and Porterville are licensed hospitals, and because their populations are full‑time patients, all interactions between staff and patients are an opportunity to provide care. Therefore, for Atascadero and Porterville, we also used the ratio of civil service employees to contract workers from the shift staffing reports to determine the level of interaction between staff and patients, and to approximate the proportion of patients that state employees and contract workers served.
Based on our review of these shift‑staffing reports, we found that state employees made up most of the workers in each shift. Specifically, as Figure 12 shows, state employees made up from 72 percent to 97 percent of the shifts when classified by the time of day, and from 78 percent to 94 percent of the shifts when classified by weekdays or weekends. Of the 126 shifts that we tested at each facility, we found that state employees worked all of them, except for two shifts at Salinas Valley in 2019, while contract workers covered some unfilled positions during 70 shifts at Atascadero, 104 shifts at Porterville, and 120 shifts at Salinas Valley.
Figure 12
State Employees Represented the Majority of the Health Care Staff on Each Shift We Reviewed at the Three Facilities From 2019 Through 2024

Source: Facility staffing logs and reports from Atascadero, Porterville, and Salinas Valley for one week at the end of April and beginning of May for each year from 2019 through 2024.
Note: This figure reflects the number of individuals who worked each shift we tested. This differs from Figure 5, which shows the number of filled positions, positions covered by state employee overtime and contract worker FTE, and uncovered vacant positions. When considered at the shift level, contract workers make up a somewhat greater—although still small—proportion of the individuals who worked when compared to overall staffing levels, because the shift staffing analysis does not account for state employee overtime or uncovered vacant positions.
Stacked column chart shows that for all three facilities, contract workers made up less than 30 percent of health care staff while state employees were the greater proportion on each shift we reviewed from 2019 through 2024.
At Atascadero, contract workers made up 3 percent of day shift health care staff, 9 percent of night shift health care staff, and 8 percent of overnight shift health care staff Additionally, contract staff worked 6 percent of weekday shifts and 8 percent of weekend shifts.
At Porterville, contract workers made up 5 percent of day shift health care staff, 8 percent of night shift health care staff, and 7 percent of overnight shift health care staff. Additionally, contract workers worked 6 percent of both weekday and weekend shifts.
At Salinas Valley, contract workers made up 19 percent of day shift health care staff, 16 percent of night shift health care staff, and 28 percent of overnight shift health care staff. Additionally, contract staff worked 19 percent of weekdays shifts and 22 percent of and weekend shifts.
We also attempted to obtain patient‑provider visit data from each facility for further analysis of the number of patients seen by state employees and contract workers, but only Salinas Valley was able to provide data that would allow for this type of analysis. Our analysis of Salinas Valley’s data further supported our review of the shift‑staffing reports that most patients were served by state employees.
We Interviewed Frontline Staff to Identify Their Workplace Concerns
The Audit Committee directed us to evaluate the facilities’ provision of patient care and to assess notable trends in areas such as vacancies, staff recruiting, and hiring. To address these areas of interest, we conducted structured interviews with a selection of frontline state employees and contract workers at Atascadero, Porterville, and Salinas Valley.11 We present our results aggregated together, rather than by facility, to allow participants to remain anonymous. We summarize the responses we received in Table 12.
Recommendations
Legislature
To maximize the effectiveness of the State’s recruiting efforts, the Legislature should require CalHR to assemble and coordinate a cross‑agency collaborative campaign to recruit medical and mental health care staff for state facilities statewide. CalHR should continue, modify, and improve such efforts until the State can achieve and maintain appropriate vacancy rates, as the Legislature determines. This campaign should include, but not be limited to, the following:
- A total compensation analysis, and adjust as appropriate, to ensure that all medical and mental health care classifications’ compensation is commensurate and competitive with similarly situated recruiting entities.
- The provision of online and in‑person assistance for candidates during the application and testing process.
- The implementation of targeted efforts, including development of marketing materials, as appropriate, highlighting the benefits of state employment in California, to recruit candidates for specific job classifications and facility locations that are historically difficult to fill.
- The establishment of measurement metrics to track the results of each type of recruiting activity and test modifications to each strategy. These measurements should include, but not be limited to, the number of candidates who express interest, apply, interview, receive, and accept employment offers.
CDCR
To improve Salinas Valley’s ability to recruit and retain medical and mental health care employees, CDCR should, by June 2026, do the following:
- Develop and implement a process to measure the effectiveness of each of its recruiting strategies and track those strategies’ costs.
- Evaluate whether offering affordable housing options would improve Salinas Valley’s ability to recruit new state employees, and if so, explore options to develop or obtain additional affordable housing units for Salinas Valley’s staff and seek a funding allocation from the Legislature to do so.
By December 2026, CDCR with Salinas Valley should comprehensively assess the technical, financial, legal, and operational impacts of implementing flexible shifts, including but not limited to, 8‑, 10‑, and 12‑hour shift options for staff. Using the results of this assessment, they should develop concrete plans to address employee concerns related to scheduling flexibility to the extent feasible.
To ensure transparency, increase accountability, and allow adequate oversight, CDCR should immediately require its facilities to establish a system to track, tabulate, periodically report to CDCR, and make publicly available the following:
- Staffing levels by shift, including the individuals’ classifications and whether they are state employees or contract workers.
- The number of shifts during which and the number of staff by which the facility fell short of its required shift‑staffing minimums, as well as an explanation for why it missed the minimums.
DDS
To improve Porterville’s ability to recruit and retain medical and mental health care employees, DDS should do the following:
- With Porterville, develop and implement a process by June 2026 to measure the effectiveness of their recruiting strategies and track those strategies’ costs.
- To ensure that Porterville is competitive in the marketplace for health care professionals, conduct a salary survey, by December 2026, that compares the salaries and benefits it offers its health care workers to those offered by local public health care facilities, private health care facilities, and staffing agencies. DDS should use this survey in its discussions with CalHR and Finance.
- By June 2026, pilot and consider permanently implementing one‑ to three‑day recruiting events that allow candidates to apply, interview, and receive a conditional job offer before the event’s conclusion.
- Evaluate by June 2026 whether offering affordable housing options would improve Porterville’s ability to recruit new state employees, and if so, explore options to develop or obtain additional affordable housing units for Porterville’s staff and seek a funding allocation from the Legislature to do so.
By December 2026, DDS with Porterville should comprehensively assess the technical, financial, legal, and operational impacts of implementing flexible shifts, including but not limited to, 8‑, 10‑, and 12‑hour shift options for staff. Using the results of this assessment, they should develop concrete plans to address employee concerns related to scheduling flexibility to the extent feasible.
To ensure that its proposed budget accurately reflects its facilities’ operational needs, DDS should, by June 2026, develop comprehensive policies and procedures for its annual budgeting process that include the requirement that staff use appropriate models to evaluate facility staffing needs and seek adjustments to position authority as necessary.
To ensure transparency, increase accountability, and allow adequate oversight, DDS should immediately require its facilities to establish a system to track, tabulate, periodically report to DDS, and make publicly available the following:
- Staffing levels by shift, including the individuals’ classifications and whether they are state employees or contract workers.
- The number of shifts during which and the number of staff by which the facility fell short of its required shift‑staffing minimums, as well as an explanation for why it missed the minimums.
DSH
To improve Atascadero’s ability to recruit and retain medical and mental health care employees, DSH should do the following:
- With Atascadero, develop and implement a process by June 2026 to measure the effectiveness of their recruiting strategies and track those strategies’ costs.
- To ensure that Atascadero is competitive in the marketplace for health care professionals, conduct a salary survey, by December 2026, that compares the salaries and benefits it offers its health care workers to those offered by local public health care facilities, private health care facilities, and staffing agencies. DSH should use this survey in its discussions with CalHR and Finance.
- By June 2026, pilot and consider permanently implementing one‑ to three‑day recruiting events that allow candidates to apply, interview, and receive a conditional job offer before the event’s conclusion.
- Evaluate by June 2026 whether offering affordable housing options would improve Atascadero’s ability to recruit new state employees, and if so, explore options to develop or obtain additional affordable housing units for Atascadero’s staff and seek a funding allocation from the Legislature to do so.
By December 2026, DSH with Atascadero should comprehensively assess the technical, financial, legal, and operational impacts of implementing flexible shifts, including but not limited to, 8‑, 10‑, and 12‑hour shift options for staff. Using the results of this assessment, they should develop concrete plans to address employee concerns related to scheduling flexibility to the extent feasible.
To ensure that its proposed budget accurately reflects its facilities’ operational needs, DSH should, by June 2026, develop comprehensive policies and procedures for its annual budgeting process that include the requirement that staff use appropriate models to evaluate facility staffing needs and seek adjustments to position authority as necessary.
To ensure transparency, increase accountability, and allow adequate oversight, DSH should immediately require its facilities to establish a system to track, tabulate, periodically report to DSH, and make publicly available the following:
- Staffing levels by shift, including the individuals’ classifications and whether they are state employees or contract workers.
- The number of shifts during which and the number of staff by which the facility fell short of its required shift‑staffing minimums, as well as an explanation for why it missed the minimums.
We conducted this performance audit in accordance with generally accepted government auditing standards and under the authority vested in the California State Auditor by Government Code section 8543 et seq. Those standards require that we plan and perform the audit to obtain sufficient, appropriate evidence to provide a reasonable basis for our findings and conclusions based on the audit objectives. We believe that the evidence obtained provides a reasonable basis for our findings and conclusions based on our audit objectives.
Respectfully submitted,
GRANT PARKS
California State Auditor
December 4, 2025
Staff:
Kris D. Patel, Audit Principal
David DeNuzzo, CIA, CFE, Senior Auditor
Rachel Adams
Danielle Bárcena, MPH, CHES
Kristen Cardon
Delise M. Coleman, MSIOP
Miles Culpepper, Ph.D
Alicen Dietrich
Nathan Drake
William Goltra
Karen Wells
Data Analytics:
Ryan Coe, MBA, CISA
Andrew Jun Lee
Grant Volk, MA, CFE
Legal Counsel:
Jacob Heninger
Appendices
Appendix A
Facility Health Care Staffing Contracts
The Audit Committee asked us to determine each facility’s current medical and mental health care worker contracts and, for each contract, to identify the contractor’s name, type of service provided, cost, and contract duration. Table A.1, Table A.2, and Table A.3 provide a list of contracts available to each of the three facilities from July 1, 2019, through June 30, 2025.12 The Audit Committee also asked us to identify the same information for contracts in the current and upcoming budget years. We include the information for contracts available for the facilities from July 1, 2025 through September 30, 2025 in Table A.4. We did not include the additional contracts we show in Table A.4 as part of our analysis in the report. For statewide contracts that were not exclusive to one facility, we showed both the overall contract amount and the projected contract amount for the facility. For Atascadero and Porterville, the facility amount shown is for the contract period. For Salinas Valley, the facility amount shown is CDCR’s allotment to the facility from fiscal years 2019–20 through 2024–25.
Appendix B
Facilities’ Vacancy Rates, Hires, and Separations Vary by Job Classification Grouping
To provide more detail about the overall vacancy rates we discuss in the report, Table B.1 shows the vacancy rate by fiscal year, position type, and facility. As we discuss in the report, the nursing grouping comprises most of each facility’s authorized positions and has the largest impact on the facilities’ overall vacancy rates.
Table B.2 shows for each facility, by fiscal year and position type, the number of state employees appointed and the number that separated, including an associated calculation of the facilities’ net gains or losses by position type and overall. Appointments include hires and changes in job classification, while separations include separations from the facility or changes in job classification—if an individual changed from one job classification to another within the same group and facility, they were counted as both an appointment and a separation, resulting in no net gain or loss in that grouping. As we discuss in the report, while the net gains and losses remained fairly steady from year to year in most groupings, they fluctuated considerably in the nursing grouping at each facility throughout our audit period.
Appendix C
Facility Vacancy Savings
Each facility budgeted funds for medical and mental health care positions that it did not fill and thus had vacancy savings. The budget staff at each department asserted that they use a portion of their vacancy savings toward the cost of contract workers, as well as other costs associated with filling vacancies, such as overtime and temporary help. However, after accounting for the cost of contract workers, each facility still had vacancy savings remaining. Table C.1, Table C.2, and Table C.3 show the vacancy savings we calculated for each facility by job classification grouping.
Appendix D
Hourly Costs for State Employees and Contract Workers
We calculated the average hourly costs each facility incurred for contract workers and state employees in a variety of medical and mental health care classifications. We found that for most classifications, contract workers cost more per hour than state employees. We included the State’s contributions for benefits and withholdings when calculating the total cost for state employees. Similarly, when calculating the total cost for contract workers, we included any administration fees or overhead paid to the staffing agency. Table D summarizes the average hourly costs per fiscal year for selected medical and mental health care classifications at the three facilities from fiscal years 2019–20 through 2024–25.
Appendix E
Results of Facility Recruiting Efforts
We evaluated the number of job applications each of the three facilities received and rejected and the number of applicants they interviewed and hired for five different job classifications from calendar years 2019 to 2024. We found that despite Salinas Valley having the overall highest number of applicants, it hired just 11 percent or fewer of those whose applications were accepted for each classification, as Table E shows. Although Atascadero and Porterville generally received fewer applications than Salinas Valley, each of these facilities hired a greater percentage of their accepted applicants. Specifically, Atascadero hired from 20 percent to 59 percent of its accepted applicants in the selected job classifications, and Porterville generally hired from 24 percent to 38 percent of its accepted applicants.
Appendix F
Scope and Methodology
The Audit Committee directed the California State Auditor to conduct an audit of the use of medical and mental health care staffing contracts by CDCR, DDS, DSH, Salinas Valley, Porterville, and Atascadero. Specifically, the Audit Committee directed us to review the three facilities’ use of contract workers, their health care staff vacancies, and their oversight of staffing levels. Table F lists the objectives that the Audit Committee approved and the methods we used to address them. Unless otherwise stated in the table or elsewhere in the report, statements and conclusions about items selected for review should not be projected to the population.
Assessment of Data Reliability
The U.S. Government Accountability Office, whose standards we are statutorily obligated to follow, requires us to assess the sufficiency and appropriateness of computer‑processed information we use to support our findings, conclusions, or recommendations. In performing this audit, we relied on payment and employment history data that we obtained from the California State Controller’s Office (SCO), position vacancy data obtained from the SCO and Porterville, as well as contractor invoice data and patient and provider data we obtained from CDCR. To assess the reliability of these data, we reviewed existing information about the data systems, interviewed people knowledgeable about the data, performed dataset verification, and performed electronic testing of key data elements. We also performed completeness and accuracy testing of CDCR’s contractor invoice data. As a result of this testing, we found the SCO’s payment and employment history data and CDCR’s contractor invoice data to be sufficiently reliable to support our findings, conclusions, and recommendations. However, we found CDCR’s patient and provider data, as well as SCO’s and Porterville’s position vacancy data to be of undetermined reliability. Although we recognize that limitations in these data may affect the precision of the numbers we present, there is sufficient evidence in total to support our audit findings, conclusions, and recommendations.
Responses
- California Department of Corrections and Rehabilitation
- Department of Developmental Services
- Department of State Hospitals
California Department of Corrections and Rehabilitation
November 14, 2025
Mr. Grant Parks
California State Auditor
621 Capitol Mall, Suite 1200
Sacramento, CA 95814
Dear Mr. Parks:
Thank you for the opportunity to review the 2024-114 – Confidential Draft Audit Report regarding the use of medical and mental health care staffing contracts by the California Department of Corrections and Rehabilitation (CDCR) and Salinas Valley State Prison. CDCR is committed to providing adequate health care for the incarcerated population, while ensuring fiscal responsibility. We appreciate your time and collaboration on this important topic.
Sincerely,
JEFF MACOMBER
Secretary
Department of Developmental Services
November 14, 2025
Grant Parks
California State Auditor
621 Capitol Mall, Suite 1200
Sacramento, CA 95814
SUBJECT: 2024-114—DRAFT REPORT RESPONSE
Dear Grant Parks:
The Department of Developmental Services (Department) has reviewed the California State Auditor’s (CSA) report entitled “State Health Care Staffing Contracts”. The Department appreciates the opportunity to respond to the report and provide comments. This response to the audit report does not address the audit’s recommendations that are directed to other state departments and the Legislature.
The Department takes pride in our employees’ care and supervision of the people entrusted to us. There are many state job classifications involved in that care and supervision, ranging across janitorial, law enforcement, administrative, clinical, and healthcare employees. We appreciate the report’s recognition that contracted medical and mental health services are a very small percentage of the overall staffing expenditure for Porterville Developmental Center (Porterville).
Despite this small percentage, contracted staff have a vital role in avoiding gaps in our ability to provide that care and supervision. During the COVID-19 pandemic, which was a large part of the time period covered by this audit’s scope, this contracted staff was able to fill in behind state staff that became ill, provide surge capacity and mitigate COVID-19 outbreaks among residents. In cautiously erring on the side of appropriately and timely protecting residents and staff at Porterville, contracts for medical and mental health staff were sizable. However, as noted in the audit report, the actual expenditures pursuant to these contracts were significantly smaller than the total amounts authorized by those contracts.
The Department continues to recognize the importance of having a qualified and stable workforce across all employee classifications to serve individuals with intellectual and developmental disabilities. We concur with statements within the audit report that contracted staff are more expensive than state staff; can achieve less familiarity with Porterville, its residents, and the care program’s design; and usually cannot develop meaningful long-term relationships and understanding of individual Porterville residents. The Department is committed to continuous improvement in recruiting and retaining employees, not just health care and mental health professionals, to help maintain appropriate staffing levels at Porterville.
The Department generally accepts the audit findings and intent of its recommendations, which are individually addressed in the attachment to this letter. On behalf of the Department, I would like to thank your audit team for its evaluation of the Department’s use of contracted employees. The findings and recommendations in the audit report support our ongoing efforts to deliver upon the promises of the Lanterman Act for the individuals we serve.
Sincerely,
PETER CERVINKA
Director
Attachment
This Attachment responds to each recommendation directed to the Department of Developmental Services:
To improve Porterville’s ability to recruit and retain medical and mental health care employees, DDS should do the following:
- With Porterville, develop and implement a process by June 2026 to measure the effectiveness of their recruiting strategies and track those strategies’ costs.
The Department agrees that identifying the most effective recruitment strategies is important, with a cost-effectiveness lens too. Given the large ongoing vacancy rates at Porterville, the Department will continue its wide-ranging recruitment efforts, which are described in the report. These include, and are not limited to, funding community college events, engaging local high school students, online job listing services, community events, and inclusion of job opportunities in the Department’s monthly newsletter to thousands of people. The Department commits to developing a process for tracking all of the Department’s recruitment costs, not just at Porterville, by June 2026. - To ensure that Porterville is competitive in the marketplace for health care professionals, conduct a salary survey, by December 2026, that compares the salaries and benefits it offers its health care workers to those offered by local public health care facilities, private health care facilities, and staffing agencies. DDS should use this survey in its discussions with CalHR and Finance.
① The Department agrees with the intent of this recommendation. However, formal salary surveys typically are conducted by the California Department of Human Resources (CalHR). As noted in the report, the Department’s historical and current experience with recruitment and retention suggests there are opportunities to improve parity with public and private entities performing similar services, and not just for medical and mental health professions. - By June 2026, pilot and consider permanently implementing one- to three-day recruiting events that allow candidates to apply, interview, and receive a conditional job offer before the event’s conclusion.
We concur with the intent of this recommendation, and further suggest that broader updates to the State’s recruitment process would be helpful. Of note, Assembly Bill 313 (Chapter 515, Statutes of 2021) requires a report to the Legislature from the Government Operations Agency at the end of December 2025, which we expect will include multiple recommendations that would be applicable beyond that report’s focus on the employment by the State of people with disabilities.
Within the constraints of the State’s civil service merit system, the Department already has been attempting to shorten the time between an indication of job applicant interest and a formal job offer. ② The Department has conducted several such multi-day events, offering education, application process guidance, and informal discussions about specific job opportunities. As human resources functions are consolidated within the Department by the end of June 2026, there will be more support available to Porterville, Canyon Springs, and other state-operated facility locations to conduct such events. - Evaluate by June 2026 whether offering affordable housing options would improve Porterville’s ability to recruit new state employees, and if so, explore options to develop or obtain additional affordable housing units for Porterville’s staff and seek a funding allocation from the Legislature to do so.
The Department concurs that affordable housing is helpful with recruitment. ③ However, employee housing available from the Department itself relies upon existing buildings at the Porterville site, and is not the product of new development which can be costly and take significant time to make habitable. Consistent with Recommendation #1 above, the Department does not believe this is a cost-effective recruitment strategy, despite its obvious benefits. Should the Legislature choose to appropriate funding for this purpose, however, the benefits of such housing could be realized over the long-term. - By December 2026, DDS with Porterville should comprehensively assess the technical, financial, legal, and operational impacts of implementing flexible shifts, including but not limited to, 8-, 10-, 12-hour shift options for staff. Using the results of this assessment, they should develop concrete plans to address employee concerns related to scheduling and flexibility to the extent feasible.
The Department agrees that flexible shift durations could assist some employees and potentially stress other employees. Changes to schedules is subject to collective bargaining, and would implicate a host of other considerations including overtime costs, predictability of schedules, shift changes and associated security protocols, managing different shift durations to comply with licensing standards and care and supervision needs with necessary management flexibility. With CalHR, the Department remains committed to harmonious relations with its applicable collective bargaining representatives, inclusive of this recommendation. - To ensure that its proposed budget accurately reflects its facilities’ operational needs, DDS should, by June 2026, develop comprehensive policies and procedures for its annual budgeting process that include the requirement that staff use appropriate models to evaluate staffing needs and seek adjustments to position authority as necessary.
The Department agrees with the intent of this recommendation to assure staffing needs are met. The annual budget is constructed starting with the Supplementary Schedule of Salaries and Wages (the Department of Finance’s “Schedule 7A”), which assumes the full resident population legally allowed at all state-operated facilities. Utilization of the current budget construction methodology assures the availability of adequate resources, and historically has resulted in substantial year-end reversion of unused funding to the State’s General Fund. A substantial portion of these historical savings have been identified for ongoing budget solutions in the last two state Budget Acts. The same is true for authorized staffing, as evidenced by the high vacancy rates noted in the audit report. Despite these savings and vacancy rates, failure to maintain adequate care and supervision of Porterville residents has not been an item materially noted by the California Department of Public Health’s licensing division’s recurring monitoring visits. ④ The Department therefore is comfortable with the adequacy of current budget and staffing authorities. - To ensure transparency, increase accountability, and allow adequate oversight, DDS should immediately require its facilities to establish a system to track, tabulate, periodically report to DDS and make publicly available the following:
a. Staffing levels by shift, including classification and whether they are a state employee or contract worker.
b. The number of shifts during which and the number of staff by which the facility fell short of its required shift-staffing minimums, as well as why it missed the minimums.
⑤ Complementary to the response to Recommendation #6, the Department does not agree that this recommendation is necessary. Overall staffing is authorized and reported in the annual Budget Act, along with expenditure information. Day-to-day staffing requirements are determined by the fluctuating needs of residents, and in compliance with licensing standards.
Comments
California State Auditor’s Comments on the Response From the Department of Developmental Services
To provide clarity and perspective, we are commenting on the response to our audit report from DDS. The numbers below correspond with the numbers we have placed in the margin of DDS’s response.
① DDS’s statement that formal salary surveys are typically conducted by CalHR is incorrect. As we describe in the report, CalHR performs total compensation analyses on some state occupations, which are high-level and do not include all medical and mental health care classifications. In fact, CalHR’s deputy director of fiscal and data management explained that it is departments’ responsibility to conduct salary studies for specific classifications, which also consider their facilities’ specific geographical locations and competition. Thus, we stand by our recommendation that DDS should conduct a salary survey to ensure that Porterville is competitive in the marketplace for health care professionals.
② DDS appears to misunderstand our recommendation. In its response, DDS states that it has conducted several multi-day events at which it offered education, application guidance, and had informal discussions about specific job opportunities. Although we believe these recruitment efforts can be effective, our recommendation specifically focuses on DDS implementing events that allow candidates to apply, interview, and receive a conditional offer before the event’s conclusion. As we state in the report, CDCR has conducted such events to streamline the state civil service hiring process.
③ We question the basis for DDS’ belief that providing affordable housing options is not a cost-effective recruitment strategy given it has not conducted an evaluation of such options as we recommend. Further, as we describe in the report, Porterville at times has offered its housing facilities to newly hired employees as a recruiting strategy and staff stated that there are normally some vacancies. With the availability of affordable housing being a statewide concern, it would be prudent for Porterville to evaluate whether it could better leverage its existing housing as part of its recruiting efforts.
④ Although DDS states it is comfortable with the adequacy of its current budget and staffing authorities, we are concerned that they might not be accurate. Specifically, we describe in the report that Porterville has accumulated significant vacancy savings over the six fiscal years of our audit period. Further, as we state in the report, even after accounting for State employees’ overtime and contract workers’ hours, each of the three facilities we reviewed—including Porterville—still had a significant number of uncovered vacant positions, which calls into question why the facilities need these additional positions. Importantly, as we describe in the report, DDS’s assistant deputy director of its state-operated facilities division acknowledged that the department may be budgeting unnecessary positions and that it is currently working with Finance to align its authorized positions with its needs. Thus, we stand by our recommendation that it take the steps necessary to ensure its proposed budget accurately reflects its facilities’ operational needs.
⑤ We disagree with DDS’s position that our recommendation, which aims to ensure adequate oversight of staffing levels and required shift-staffing minimums, is unnecessary. As we state in the report, Porterville tracks some shift-staffing information, but its tracking mechanism lacks key components, such as the type of treatment to be delivered or the number of patients per shift, to demonstrate that it schedules sufficient staff to meet the required staff-to-patient ratios. Further, as we state in the report, DDS has not formally or specifically requested that facilities track, tabulate, and report their compliance with staffing minimums, nor has it developed a formal process for the facilities to do so. Without such oversight, DDS cannot be certain that its facilities are staffed appropriately for each shift to provide adequate medical and mental health care.
Department of State Hospitals
November 17, 2025
Grant Parks
California State Auditor
621 Capital Mall, Suite 1200
Sacramento, CA 95814
Dear Mr. Parks,
This letter is in response to the draft audit report, 2024-114 State Health Care Staffing Contracts. Thank you for the opportunity to review and provide a response to the recommendations presented in the report. The Department of State Hospital’s (DSH) response to the recommendations are included in the attachment. DSH also appreciates the opportunity to emphasize and clarify several aspects of its operations and the audit report:
- Safety, care and treatment are a top priority – DSH provides care and treatment to over 5,500 patients daily in a 24/7/365 setting, through its dedicated and talented treatment team and level of care nurses. The treatment team is comprised of psychiatrists, psychologists, rehabilitation therapists and social workers. The interdisciplinary treatment team works to develop a treatment plan and diagnosis, a plan for delivery of group treatment and as needed one-to-one treatment, sets treatment goals, coordinates discharge planning, and performs medication management. Roles within the level-of-care nursing category include registered nurses, licensed vocational nurses, and psychiatric technicians. Nursing services provide the essential 24-hour care necessary to treat and house patients with psychiatric needs. DSH prioritizes and values providing services through its dedicated civil service team members as evidenced in the report. ① The audit report found that DSH-Atascadero’s overall staffing levels provided were comprised of 95% civil service staff. DSH’s use of contracted staff represented a very small portion of staff delivered to fulfill the Department’s mission. Due to the nature of DSH’s operations, challenges experienced with recruitment/retention during the COVID-19 global pandemic and other factors beyond the Department’s control, DSH has supplemented staffing to maintain the necessary staffing to continuously provide quality medical and psychiatric care and treatment for its patients.
- DSH regularly meets and exceeds level of care staffing minimums –DSH’s hospitals regularly meet and exceed minimum staffing levels across all its hospitals. ② While the report notes three occurrences during the 5 year audit period where DSH-Atascadero did not meet staffing minimums, these isolated shortages were due to extraordinary circumstances when a significant surge of COVID-19 infections amongst the staff occurred during declared states of emergency. Specifically, in one instance, an unusually high numberof staff called out of their shift on a holiday (i.e., Christmas Eve) at the same time COVID-19 infections were impacting staffing levels, and in a second, a local flood prevented staff from safely reaching the facility. DSH-Atascadero self-reported each of these events to the California Department of Public Health, its applicable labor partners, and also notified the DSH Director’s Office of the situation as required by DSH policy. DSH recognizes the criticality of ensuring it meets its level of care staffing minimums as well as having appropriate departmental oversight of these instances.
- DSH offers significant schedule flexibility for its staff– In recent years, DSH has moved to provide significant scheduling flexibilities in an effort to retain its mental health and nursing staff. For mental health staff, alternate work schedules (including 4/10s and 9/8/80) and telework have been offered while balancing the direct patient treatment needs. ③ For nursing staff, the department offers both 8-hour and 12-hour shifts as well as some 9/8/80 schedules. These flexible schedules are considered and approved based on job classification, role, responsibilities, duties and operational need for a 24/7 hospital. DSH has worked collaboratively with labor unions to consider schedules that are feasible through Joint Labor Management Committee meetings, statewide pilots, ad-hoc discussions, etc.
- DSH uses approved budgeting staffing standards to adjust resources based on significant policy or programatic changes – The audit report states that “the department was unable to justify how it budgets for health care staffing”. ④ DSH and the Department of Finance (DOF) completed a mission-based-review (MBR) and established budgeting staffing standards for nursing level of care, treatment team and primary care, and forensic staffing. These staffing standards were presented to the Legislature in budget change proposals, supported by DOF, and approved along with position adjustment requests to realign positions across the hospitals where possible to meet treatment, evaluation, and care needs. Where realignments were not possible, additional positions were approved to provide hospitals the position authority needed to meet the staffing standards. Below are the details for each MBR approval:
- Fiscal Year (FY) 2019-20 – Direct Care Nursing and Court Evaluations and Reports
- Heard in the Assembly Budget Subcommittee No. 1 on Health and Human Services on 03/04/2019 and approved as budgeted
- Heard in the Senate Budget Subcommittee No. 3 on Health and Human Service on 05/02/2019 and approved as budgeted
- FY 2020-21 – Treatment Team and Primary Care
- Heard in the Assembly Budget Subcommittee No. 1 on Health and Human Services on 06/12/2020 and was deferred without prejudice. A revised proposal was ultimately approved by the Budget Committee for inclusion in the 2020 Budget Act.
- Heard in the Senate Subcommittee No. 3 on Health and Human Service on 05/24/2019 and was deferred without prejudice. A revised proposal was ultimately approved by the Budget Committee for inclusion in the 2020 Budget Act.
- Fiscal Year (FY) 2019-20 – Direct Care Nursing and Court Evaluations and Reports
As part of the Governor’s Budget and May Revise process, DSH bi-annually provides updates and/or adjustments to its staffing, using its staffing standards, based on significant policy and/or programmatic changes such as the construction of the Enhanced Treatment Program, right-sizing COVID-19 isolation unit based on utilization, and the closure of units. Each update is heard by the legislative subcommittees.
- Salary savings is overstated in the audit report: The audit report reflects greater salary savings than the department incurred during the audit scope. ⑤ The savings identified in the audit did not incorporate full costs of personnel services wages as well as other payments such as workers’ compensation, nonindustrial disability, and temporary disability, the amount of salary savings is overstated. The allocation of vacant position salary savings, as well as having flexibility within DSH’s operating expenditure budget, allowed the department to maintain mandated patient mental health services through the utilization of those dollars for overtime, temporary help, and contractors as well as emergent one-time needs that arise primarily due to infrastructure repairs or equipment replacements. Furthermore, the Department utilizes the Governor’s Budget and May Revise process to return position related savings associated with significant program changes and/or project delays.
- DSH conducts significant ongoing recruitment and retention efforts: Recruitment and retention have been historically challenging for DSH and have only been exacerbated during the pandemic. While DSH is not alone in its staffing challenge for its health care workforce, DSH does present unique challenges for recruitment and retention due to multiple factors. The individuals DSH serves have some of the most difficult to treat behavioral health challenges, some with a significant violence risk level. This, coupled with the geographic locations of DSH’s facilities and nationwide shortages for the healthcare workforce, makes recruitment and retention very challenging. ⑥ While the audit report acknowledges some of DSH’s recruitment efforts, it did not adequately describe DSH’s significant recruitment efforts. DSH has implemented a multi-faceted approach to its efforts to recruit and retain team members, specifically focused across four domains: 1) marketing/outreach; 2) streamlining the hiring process; 3) developing and expanding training programs; and 4) employee compensation. DSH-Atascadero participates in statewide recruitment initiatives such as partnering with a firm to conduct marketing recruitment campaigns, collaborating with California psychiatric technician programs to take recruitment efforts more upstream, participating regularly in virtual career fairs and hosting onsite career fairs. DSH-Atascadero has established partnerships with many educational institutions to serve as a training and clinical rotation site for various disciplines including but not limited to psychiatry, psychology, and social work. Partners include Stanford, Community Memorial Health for 4th year psychiatry residents, and specific for nursing classifications Cuesta, Cal State Monterey Bay and Allen Hancock College, which result in a direct pipeline into employment with DSH. DSH-Atascadero also continues to invest in developing its own team members through the offering of a 20/20 training program, which provides selected, qualified employees wishing to become Psychiatric Technicians, Registered Nurses or Clinical Social Worker the opportunity to participate in an approved full-time academic program while working half-time (generally 20 hours per week) in their current classification while receiving full pay and benefits.
We would like to thank your staff for their professionalism, time, and courtesy during the audit. In addition, we appreciate the recognition of the challenges presented when staffing a 24/7/365 hospital system, particularly during a multi-year global pandemic as well as the recommendations to assist DSH with its recruitment and retention initiatives.
Please contact Liliana Lopez, Chief of the Office of Audits, at liliana.lopez@dsh.ca.gov if you have any questions.
Sincerely,
Stephanie Clendenin
Director
Department of State Hospitals
Response to the California State Auditor
Draft Report Entitled: State Health Care Staffing Contracts
Recommendation 1: To improve Atascadero’s ability to recruit and retain medical and mental health care employees, DSH should do the following:
- With Atascadero, develop and implement a process by June 2026 to measure the effectiveness of their recruiting strategies and track those strategies’ costs.
- To ensure that Atascadero is competitive in the marketplace for health care professionals, conduct a salary survey by December 2026 that compares the salaries and benefits it offers its health care workers to those offered by local public health care facilities, private health care facilities, and staffing agencies. DSH should use this survey in its discussions with CalHR and Finance.
- By June 2026, pilot and consider permanently implementing one- to three-day recruiting events that allow candidates to apply, interview, and receive a conditional job offer before the event’s conclusion.
- Evaluate by June 2026 whether offering affordable housing options would improve Atascadero’s ability to recruit new state employees, and if so, explore options to develop or obtain additional affordable housing units for Atascadero’s staff and seek a funding allocation from the Legislature to do so.
Response: Partially Agree
DSH will implement the following recommendations:
- By June 2026, develop and implement a process to measure the effectiveness of DSH-Atascadero’s recruitment strategies including cost.
- By December 2026, DSH will conduct a salary survey.
- By June 2026, pilot and evaluate the effectiveness of 1-3 day recruiting events. DSH notes that it has already piloted and implemented same-day hiring events at other hospitals including DSH-Atascadero, however, DSH-Atascadero has not conducted this type of event specific to the classifications included in this audit. It is important to note, however, that based on the results of other same-day hiring events across the DSH-system, the success in both candidate interest and successful contingent offers is higher for entry level classifications such as analyst, food service technicians, and custodians with less candidate interest and fewer offers made to the classifications requiring professional licensure such as psychiatry and psychology.
⑦ However, DSH disagrees with the following recommendation and provides the following additional information:
- DSH disagrees with the recommendation of evaluating whether additional affordable housing units would improve recruitment as well as seeking funding to develop such housing units. DSH-Atascadero currently provides 17 studio apartment units and 8 single rooms with communal kitchen, and bathrooms for rent to its staff on a temporary basis. This benefit is included in active job advertisements to assist as a recruitment tool. The recommendation to assess whether additional housing units would improve recruitment is pre-mature as there is currently a project to develop affordable housing on the front part of the campus in accordance with Executive Order N-06-19. While this project is not led by DSH or exclusive to serving DSH-Atascadero staff, there may be the opportunity for staff to obtain access to the additional housing. In the broader context of DSH’s development of major capital outlay infrastructure proposals, DSH has other infrastructure needs across DSH-Atascadero and the entire hospital system and must prioritize evaluating and submitting proposals associated with critical infrastructure projects, including those impacting patient housing units. These have included projects such as roof projects, water and wastewater treatment, anti-ligature risks, and electrical infrastructure.
Recommendation 2: By December 2026, DSH with Atascadero should comprehensively assess the technical, financial, legal, and operational impacts of implementing flexible shifts, including but not limited to, 8-, 10-, and 12-hour shift options for staff. Using the results of this assessment, they should develop concrete plans to address employee concerns related to scheduling flexibility to the extent feasible.
Response: Partially Agree
③ By December 2026, DSH will evaluate whether it is feasible to implement additional flexible shift options for its level of care nursing staff. DSH already offers significant schedule flexibility for all of its treatment team and primary care positions, as DSH offers alternative work week schedules which may include four 10 hour shifts and 9/8/80 schedules. Additionally, the treatment team classifications have the opportunity to telework one day a week. Offering 12 hour schedules for clinicians would significantly reduce the number of clinicians M-F and would significantly impact direct patient care. For level of care, while it already provides significant flexibility, DSH will evaluate to identify if it is feasible to offer additional flexible shifts. Currently DSH- Atascadero has 220 nursing staff on a 12-hour shift, three (3) on a 10-hour shift schedule and 33 nursing staff scheduled for 9/8/80 schedules. DSH has offered some additional shifts, but not all of them have been filled/bid on by staff, and DSH and California Association of Psychiatric Technicians (BU18) have discussed this issue. Furthermore, DSH-Napa has recently implemented an alternative shift schedule that DSH can evaluate after it has been implemented for a period of time to determine if it may merit expansion to DSH-Atascadero. The department and DSH-Atascadero has demonstrated its commitment to flexible scheduling while balancing operational needs, but will evaluate to determine if there are further flexible shifts that can be offered for its nursing staff.
Recommendation 3: To ensure that its proposed budget accurately reflects its facilities’ operational needs, DSH should, by June 2026, develop comprehensive policies and procedures for its annual budgeting process that include the requirement that staff use appropriate models to evaluate facility staffing needs and seek adjustments to position authority as necessary.
Response: Agree.
DSH will implement the recommendation. DSH will develop comprehensive policies and procedures, including a requirement and process to use the staffing standard approved by the Legislature in DSH’s staffing study budget change proposals to annually evaluate its staffing to determine if there are any adjustments that may need to be considered.
Recommendation 4: To ensure transparency, increase accountability, and allow adequate oversight, DSH should immediately require its facilities to establish a system to track, tabulate, periodically report to DSH, and make publicly available the following information:
- Staffing levels by shift, including the individuals’ classification and whether they are state employees or contract workers
- The number of shifts during which and the number of staff by which the facility fell short of its required shift-staffing minimums, as well as an explanation for why it missed the minimums.
⑧ Response: Partially Agree
DSH already requires its facilities, by policy, to report to the Director’s Office, any events that are reportable to the California Department of Public Health. Reportable events would include when a hospital does not meet minimum staffing levels for a shift. However, DSH will develop a policy that explicitly describes the required minimum staffing levels and affirms the requirement that each hospital not only immediately report if they were unable to meet a shift, but to also track and periodically report data. This reporting requirement will include some level of information about the staffing levels, the number of shifts during which licensing minimums were not met, and the number of staff by which the facility fell short of its required shift-staffing licensing minimums, as well as an explanation for why it missed the minimums.
⑧ We are continuing to review this recommendation and evaluating the ability for our system to analyze staffing data in a way that it is consumable to inform quick management action and decision making. There was not sufficient time during the 5-day review period to effectively assess DSH’s resources and data capabilities. DSH will work with its hospitals and Technology Services Division to identify its data and reporting capabilities to produce a report that is consistent with the intent to provide data to increase oversight, accountability and transparency. Both policy development and reporting assessment and development will require time and cannot be accomplished immediately, as recommended. DSH anticipates it can have this work completed by June 2026.
Comments
California State Auditor’s Comments on the Response From the Department of State Hospitals
To provide clarity and perspective, we are commenting on the response to our audit report from DSH. The numbers below correspond with the numbers we have placed in the margin of DSH’s response.
① Nowhere in our report do we conclude that Atascadero’s overall staffing levels were comprised of 95 percent civil service staff, as DSH incorrectly claims in its response.
② DSH incorrectly indicates that our report concludes that Atascadero did not meet staffing minimums on three occurrences during our audit period. Rather, that was an assertion, which we include in the report, from Atascadero’s executive director. However, as we describe in the same section of the report, Atascadero does not have a formal process to tabulate the number of times it missed staffing minimums; therefore, it was unable to demonstrate to us that it did not fall short of the staffing minimums on more than three occurrences.
③ We acknowledge in the report that Atascadero offers flexible shift options for some staff, and some limited flexibility for its nursing positions. However, the fact remains that it does not offer such flexibility for all medical and mental health staff. Nonetheless, DSH agreed with our recommendation to evaluate whether it is feasible to offer additional flexible shifts for level-of-care staff, and to consider whether alternative shift schedules recently implemented at its Napa facility would merit expansion to Atascadero. We look forward to reviewing DSH’s responses to our recommendation as part of our regular follow-up process.
④ DSH’s response obfuscates our finding and recommendation. As we state in the report, DSH could not justify that its staffing level was sufficient or necessary because it does not review its staffing needs for all medical and mental health positions annually. We acknowledge that DSH developed a staffing model in 2019 that it used to support two legislatively-approved budget requests during our audit period. However, as we state in the report, DSH’s director explained that although the department could use this staffing model to evaluate all medical and mental health care staffing needs annually, it has not done so. Budgeting staff positions consistently and appropriately is critical to ensuring that the departments can request the Legislature to approve the appropriate number of necessary positions. As such, we stand by our recommendation.
⑤ DSH incorrectly claims that our report overstates salary savings. As we indicate in our scope and methodology, we determined each facility’s vacancy savings for medical and mental health care job classifications using information from the wages and salary budget supplements the departments included in their annual state budgets, and expenditure records from the SCO. Because the budget supplements generally include only salary and wages and do not include costs such as retirement contributions, employee health benefits, and worker’s compensation, we excluded these additional costs when we calculated the amount the facilities spent. In Table 11 and Table C.1, we indicate those costs we included and excluded from our calculations. Finally, as we state in the report, DSH’s budget staff asserted that DSH generally used vacancy savings to offset the costs associated with staff overtime and contract workers, as well as to pay for expenses such as equipment and special repairs.
⑥ For brevity and readability, we do not discuss the entirety of DSH’s recruitment efforts in our report. However, we acknowledge in the report that Atascadero has made significant efforts to recruit medical and mental health care professionals through various means. We also note in the report that DSH’s recruitment unit manager stated that it has successfully run a streamlined recruiting event for some facility support positions at Atascadero, and that DSH is open to expanding streamlined recruiting events to recruit for certain medical and mental health care positions.
⑦ It is unclear why DSH disagrees with our recommendation. As we state in the report, Atascadero has housing available that it has at times offered to newly hired employees as a recruiting strategy. However, Atascadero has not explored this option to attract more candidates for the facility. If implemented, our recommendation would allow Atascadero to better understand if offering housing would improve its ability to recruit new employees before deciding on whether to seek additional funding. As such, we stand by our recommendation.
⑧ We look forward to reviewing DSH’s efforts to implement this recommendation as part of our regular follow-up process.
Footnotes
- According to the bill that lowered the population cap to 211 persons, it was the intent of the Legislature that General Fund savings derived from the closure of developmental centers benefit persons with developmental disabilities living in the community. ↩︎
- CDCR is able to offer some pay differentials that other departments cannot offer due to its ongoing involvement in federal litigation. CalHR defines a pay differential as compensation in addition to base pay that is typically provided to employees in a specific class to recognize unique skill sets, circumstances, or working conditions. ↩︎
- DSH staff stated that they are piloting a recruiting software system but are not yet using the system to analyze data at the facility level. CDCR’s deputy director of human resources stated that the department began tracking the results of its recruiting strategies in late 2024, but the data are still not available. ↩︎
- We projected the number of hours worked in fiscal year 2024–25 based on actual data from July through December 2024. ↩︎
- In addition to having its own contracts, Atascadero also used staffing contracts executed by other departments during the COVID‑19 pandemic. ↩︎
- Although many of the contracts cover multiple years, the facilities and their respective departments project the usage of the contracts by fiscal year. DSH and DDS maintain documentation recording how much of the total contract value they have projected for each fiscal year and each facility. According to Porterville staff, they divide the value of the facility’s contracts equally by fiscal year, which allowed us to calculate the projected value for each fiscal year using the effective dates of the contract and the total value. According to CDCR’s former deputy director of business services, CDCR allots funds for Salinas Valley’s projected contract usage each fiscal year, but this value is not tied to the contract maximum value. ↩︎
- To determine the facilities’ average hourly costs for contract workers, we used invoice data from each facility with any additional overhead costs the facility paid. For state employees, we used payroll data from the SCO and included the State’s contributions for benefits and withholdings as well as its administrative costs. We did not include other payments such as overtime or bonuses in our analysis. Although in many cases an hour of regular pay for a contract worker would be less than an hour of overtime for a state employee, we were unable to determine how frequently this substitution occurred. We also found that contract workers frequently worked overtime, which would typically cost more than a similar amount of overtime by a state employee, possibly negating any savings. Therefore, we limited our analysis to base hourly rates. ↩︎
- We measured the tenure of state employees and contract workers who worked at the facilities between July 2019 and December 2024 by determining their employment history at the facility within a classification group between July 2019 and December 2024. ↩︎
- Mary Halter et al., “The Determinants and Consequences of Adult Nursing Staff Turnover: A Systematic Review of Systematic Reviews,” BMC Health Services Research, 17:824, 2017. https://doi.org/10.1186/s12913-017-2707-0, accessed on October 8, 2025. ↩︎
- Katie Boston‑Leary et al., “Patient Safety Amid Nursing Workforce Challenges,” Patient Safety Network, Agency for Healthcare Research and Quality, 2024, https://psnet.ahrq.gov/perspective/patient-safety-amid-nursing-workforce-challenges, accessed on August 28, 2025. ↩︎
- Structured interviews using a standardized set of interview questions allow individual testimonial data to be prepared and analyzed into a higher form of evidence through systematic analysis. ↩︎
- In some instances, the contracts began before or ended after the time period listed. However, they were in effect for at least a portion of the audit period. ↩︎